By Silvia Aloisi, Deena Beasley, Gabriella Borter, Thomas Escritt and Kate Kelland
BERLIN (Reuters) – When he was diagnosed with COVID-19, Andre Bergmann knew exactly where he wanted to be treated: the Bethanien hospital lung clinic in Moers, near his home in northwestern Germany.
The clinic is known for its reluctance to put patients with breathing difficulties on mechanical ventilators – the kind that involve tubes down the throat.
The 48-year-old physician, father of two and aspiring triathlete worried that an invasive ventilator would be harmful. But soon after entering the clinic, Bergmann said, he struggled to breathe even with an oxygen mask, and felt so sick the ventilator seemed inevitable.
Even so, his doctors never put him on a machine that would breathe for him. A week later, he was well enough to go home.
Bergmann’s case illustrates a shift on the front lines of the COVID-19 pandemic, as doctors rethink when and how to use mechanical ventilators to treat severe sufferers of the disease – and in some cases whether to use them at all. While initially doctors packed intensive care units with intubated patients, now many are exploring other options.
Machines to help people breathe have become the major weapon for medics fighting COVID-19, which has so far killed more than 183,000 people. Within weeks of the disease’s global emergence in February, governments around the world raced to build or buy ventilators as most hospitals said they were in critically short supply.
Germany has ordered 10,000 of them. Engineers from Britain to Uruguay are developing versions based on autos, vacuum cleaners or even windshield-wiper motors. U.S. President Donald Trump’s administration is spending $2.9 billion for nearly 190,000 ventilators. The U.S. government has contracted with automakers such as General Motors Co and Ford Motor Co as well as medical device manufacturers, and full delivery is expected by the end of the year. Trump declared this week that the U.S. was now “the king of ventilators.”
However, as doctors get a better understanding of what COVID-19 does to the body, many say they have become more sparing with the equipment.
Reuters interviewed 30 doctors and medical professionals in countries including China, Italy, Spain, Germany and the United States, who have experience of dealing with COVID-19 patients. Nearly all agreed that ventilators are vitally important and have helped save lives. At the same time, many highlighted the risks from using the most invasive types of them – mechanical ventilators – too early or too frequently, or from non-specialists using them without proper training in overwhelmed hospitals.
Medical procedures have evolved in the pandemic as doctors better understand the disease, including the types of drugs used in treatments. The shift around ventilators has potentially far-reaching implications as countries and companies ramp up production of the devices.
GRAPHIC: Ventilators: a bridge between life and death? – https://graphics.reuters.com/HEALTH-CORONAVIRUS/VENTILATORS/oakvekyxvrd/index.html
“BETTER RESULTS”
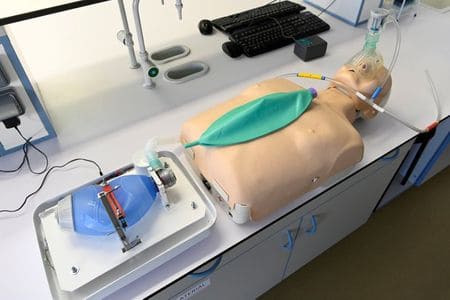
Many forms of ventilation use masks to help get oxygen into the lungs. Doctors’ main concern is around mechanical ventilation, which involves putting tubes into patients’ airways to pump air in, a process known as intubation. Patients are heavily sedated, to stop their respiratory muscles from fighting the machine.
Those with severe oxygen shortages, or hypoxia, have generally been intubated and hooked up to a ventilator for up to two to three weeks, with at best a fifty-fifty chance of surviving, according to doctors interviewed by Reuters and recent medical research. The picture is partial and evolving, but it suggests people with COVID-19 who have been intubated have had, at least in the early stages of the pandemic, a higher rate of death than other patients on ventilators who have conditions such as bacterial pneumonia or collapsed lungs.
This is not proof that ventilators have hastened death: The link between intubation and death rates needs further study, doctors say.
In China, 86% of 22 COVID-19 patients didn’t survive invasive ventilation at an intensive care unit in Wuhan, the city where the pandemic began, according to a study published in The Lancet in February. Normally, the paper said, patients with severe breathing problems have a 50% chance of survival. A recent British study found two-thirds of COVID-19 patients put on mechanical ventilators ended up dying anyway, and a New York study found 88% of 320 mechanically ventilated COVID-19 patients had died.
More recently, none of the eight patients who went on ventilators at the Cleveland Clinic Abu Dhabi hospital had died as of April 9, a doctor there told Reuters. And one ICU doctor at Emory University Hospital in Atlanta said he had had a “good” week when almost half the COVID-19 patients were successfully taken off the ventilator, when he had expected more to die.
The experiences can vary dramatically. The average time a COVID-19 patient spent on a ventilator at Scripps Health’s five hospitals in California’s San Diego County was just over a week, compared with two weeks at the Hadassah Ein Kerem Medical Center in Jerusalem and three at the Universiti Malaya Medical Centre in the Malaysian capital Kuala Lumpur, medics at the hospitals said.
In Germany, as patient Bergmann struggled to breathe, he said he was getting too desperate to care.
“There came a moment when it simply no longer mattered,” he told Reuters. “At one point I was so exhausted that I asked my doctor if I was going to get better. I was saying, if I had no children or partner then it would be easier just to be left in peace.”
Instead of putting Bergmann on a mechanical ventilator, the clinic gave him morphine and kept him on the oxygen mask. He’s since tested free of the infection, but not fully recovered. The head of the clinic, Thomas Voshaar, a German pulmonologist, has argued strongly against early intubation of COVID-19 patients. Doctors including Voshaar worry about the risk that ventilators will damage patients’ lungs.
The doctors interviewed by Reuters agreed that mechanical ventilators are crucial life-saving devices, especially in severe cases when patients suddenly deteriorate. This happens to some when their immune systems go into overdrive in what is known as a “cytokine storm” of inflammation that can cause dangerously high blood pressure, lung damage and eventual organ failure.
The new coronavirus and COVID-19, the disease the virus causes, have been compared to the Spanish flu pandemic of 1918-19, which killed 50 million people worldwide. Now as then, the disease is novel, severe and spreading rapidly, pushing the limits of the public health and medical knowledge required to tackle it.
When coronavirus cases started surging in Louisiana, doctors at the state’s largest hospital system, Ochsner Health, saw an influx of people with signs of acute respiratory distress syndrome, or ARDS. Patients with ARDS have inflammation in the lungs which can cause them to struggle to breathe and take rapid short breaths.
“Initially we were intubating fairly quickly on these patients as they began to have more respiratory distress,” said Robert Hart, the hospital system’s chief medical officer. “Over time what we learned is trying not to do that.”
Instead, Hart’s hospital tried other forms of ventilation using masks or thin nasal tubes, as Voshaar did with his German patient. “We seem to be seeing better results,” Hart said.
CHANGED LUNGS
Other doctors painted a similar picture.
In Wuhan, where the novel coronavirus emerged, doctors at Tongji Hospital at the Huazhong University of Science and Technology said they initially turned quickly to intubation. Li Shusheng, head of the hospital’s intensive care department, said a number of patients did not improve after ventilator treatment.
“The disease,” he explained, “had changed their lungs beyond our imagination.” His colleague Xu Shuyun, a doctor of respiratory medicine, said the hospital adapted by cutting back on intubation.
Luciano Gattinoni, a guest professor at the Department of Anaesthesiology, Emergency and Intensive Care Medicine, University of Göttingen in Germany, and a renowned expert in ventilators, was one of the first to raise questions about how they should be used to treat COVID-19.
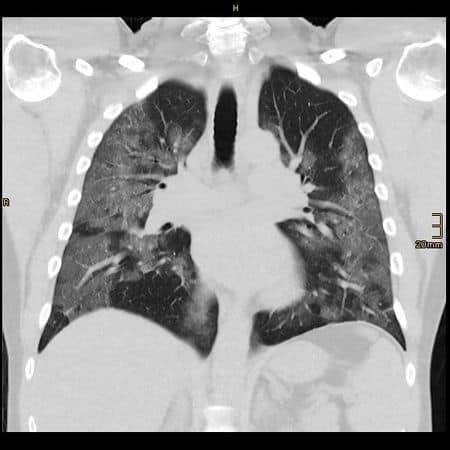
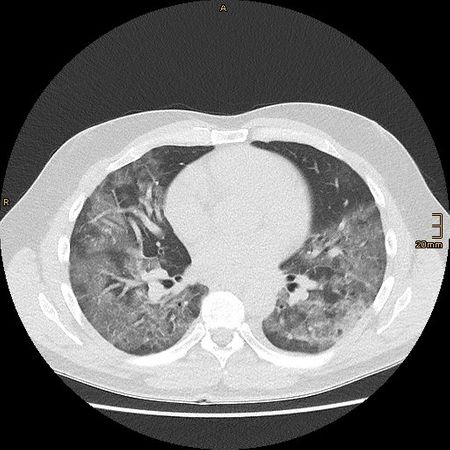
“I realised as soon as I saw the first CT scan … that this had nothing to do with what we had seen and done for the past 40 years,” he told Reuters.
In a paper published by the American Thoracic Society on March 30, Gattinoni and other Italian doctors wrote that COVID-19 does not lead to “typical” respiratory problems. Patients’ lungs were working better than they would expect for ARDS, they wrote – they were more elastic. So, he said, mechanical ventilation should be given “with a lower pressure than the one we are used to.”
Ventilating some COVID-19 sufferers as if they were standard patients with ARDS is not appropriate, he told Reuters. “It’s like using a Ferrari to go to the shop next door, you press on the accelerator and you smash the window.”
The Italians were swiftly followed by Cameron Kyle-Sidell, a New York physician who put out a talk on YouTube saying that by preparing to put patients on ventilators, hospitals in America were treating “the wrong disease.” Ventilation, he feared, would lead to “a tremendous amount of harm to a great number of people in a very short time.” This remains his view, he told Reuters this week.
When Spain’s outbreak erupted in mid-March, many patients went straight onto ventilators because lung X-rays and other test results “scared us,” said Delia Torres, a physician at the Hospital General Universitario de Alicante. They now focus more on breathing and a patient’s overall condition than just X-rays and tests. And they intubate less. “If the patient can get better without it, then there’s no need,” she said.
In Germany, lung specialist Voshaar was also concerned. A mechanical ventilator itself can damage the lungs, he says. This means patients stay in intensive care longer, blocking specialist beds and creating a vicious circle in which ever more ventilators are needed.
Of the 36 acute COVID-19 patients on his ward in mid-April, Voshaar said, one had been intubated – a man with a serious neuro-muscular disorder – and he was the only patient to die. Another 31 had recovered.
“IRON LUNGS”
Some doctors cautioned that the impression that the rush to ventilate is harmful may be partly due to the sheer numbers of patients in today’s pandemic.
People working in intensive care units know that the mortality rate of ARDS patients who are intubated is around 40%, said Thierry Fumeaux, head of an ICU in Nyon, Switzerland, and president of the Swiss Intensive Care Medicine Society. That is high, but may be acceptable in normal times, when there are three or four patients in a unit and one of them doesn’t make it.
“When you have 20 patients or more, this becomes very evident,” said Fumeaux. “So you have this feeling – and I’ve heard this a lot – that ventilation kills the patient.” That’s not the case, he said. “No, it’s not the ventilation that kills the patient, it’s the lung disease.”
Mario Riccio, head of anaesthesiology and resuscitation at the Oglio Po hospital near Cremona in Lombardy, Italy’s worst-hit region, says the machines are the only treatment to save a COVID-19 patient in serious condition. “The fact that people who were placed under mechanical ventilation in some cases die does not undermine this statement.”
Originally nicknamed “iron lungs” when introduced in the 1920s and 1930s, mechanical ventilators are sometimes also called respirators. They use pressure to blow air – or a mixture of gases such as oxygen and air – into the lungs.
They can be set to exhale it, too, effectively taking over a patient’s entire breathing process when their lungs fail. The aim is to give the body enough time to fight off an infection to be able to breathe independently and recover.
Some patients need them because they’re losing the strength to breathe, said Yoram Weiss, director of Hadassah Ein Kerem Medical Center in Jerusalem. “It is very important to ventilate them before they collapse.” At his hospital, 24 of 223 people with COVID-19 had been put on ventilators by April 13. Of those, four had died and three had come off the machines.
AEROSOLS
Simpler forms of ventilation – face masks for example – are easier to administer. But respirator masks can release micro-droplets known as aerosols which may spread infection. Some doctors said they avoided the masks, at least at first, because of that risk.
While mechanical ventilators do not produce aerosols, they carry other risks. Intubation requires patients to be heavily sedated so their respiratory muscles fully surrender. The recovery can be lengthy, with a risk of permanent lung damage.
Now that the initial wave of COVID-19 cases has peaked in many countries, doctors have time to examine other ways of managing the disease and are fine-tuning their approach.
Voshaar, the German lung specialist, said some doctors were approaching COVID-19 lung problems as they would other forms of pneumonia. In a healthy patient, oxygen saturation – a measure of how much oxygen the haemoglobin in the blood contains – is around 96% of the maximum amount the blood can hold. When doctors check patients and see lower levels, indicating hypoxia, Voshaar said, they can overreact and race to intubate.
“We lung doctors see this all the time,” Voshaar told Reuters. “We see 80% and still do nothing and let them breathe spontaneously. The patient doesn’t feel great, but he can eat and drink and sit on the side of his bed.”
He and other doctors think other tests can help before intubation. Voshaar looks at a combination of measures including how fast the patient is breathing and their heart rate. His team are also guided by lung scans.
“HAPPY HYPOXICS”
Several doctors in New York said they too had started to consider how to treat patients, known as “happy hypoxics,” who can talk and laugh with no signs of mental cloudiness even though their oxygen might be critically low.
Rather than rushing to intubate, doctors say they now look for other ways to boost the patients’ oxygen. One method, known as “proning,” is telling or helping patients to roll over and lie on their fronts, said Scott Weingart, head of emergency critical care at Stony Brook University Medical Center on Long Island.
“If patients are left in one position in bed, they tend to desaturate, they lose the oxygen in their blood,” Weingart said. Lying on the front shifts any fluid in the lungs to the front and frees up the back of the lungs to expand better. “The position changes have radically impressive effects on the patient’s oxygen saturations.”
Weingart does recommend intubating a communicative patient with low oxygen levels if they start to lose mental clarity, if they experience a cytokine storm or if they start to really struggle to breathe. He feels there are enough ventilators for such patients at his hospital.
But for happy hypoxics, “I still don’t want these patients on ventilators, because I think it’s hurting them, not helping them.”
QUALITY, SKILL
As governments in the United States and elsewhere are scrambling to raise output of ventilators, some doctors worry the fast-built machines may not be up to snuff.
Doctors in Spain wrote to their local government to complain that ventilators it had bought were designed for use in ambulances, not intensive care units, and some were of poor quality. In the UK, the government has cancelled an order for thousands of units of a simple model because more sophisticated devices are needed.
More important, many doctors say, is that the additional machines will need highly trained and experienced operators.
“It’s not just about running out of ventilators, it’s running out of expertise,” said David Hill, a pulmonology and critical care physician in Waterbury, Connecticut, who attends at Waterbury Hospital.
Long-term ventilation management is complex, but Hill said some U.S. hospitals were trying to bring non-critical care physicians up to speed fast with webinars or even tip sheets. “That is a recipe for bad outcomes.”
“We intensivists don’t ventilate by protocol,” said Hill. “We may choose initial settings,” he said, “but we adjust those settings. It’s complicated.”
(This story was refiled to correct link to graphic; adds dropped name of hospital in section 2)
(Escritt reported from Berlin, Aloisi from Milan, Beasley from Los Angeles, Borter from New York and Kelland from London. Additional reporting: Alexander Cornwell in Abu Dhabi, Panu Wongcha-um in Bangkok, Maayan Lubell in Jerusalem, A. Ananthalakshmi and Rozanna Latif in Kuala Lumpur, Kristina Cooke in Los Angeles, Sonya Dowsett in Madrid, Jonathan Allen and Nicholas Brown in New York, John Mair in Sydney, Costas Pitas in London, David Shepardson in Washington DC, Brenda Goh in Wuhan and John Miller in; Zurich. Writing by Andrew RC Marshall and Kate Kelland; Edited by Sara Ledwith and Jason Szep)