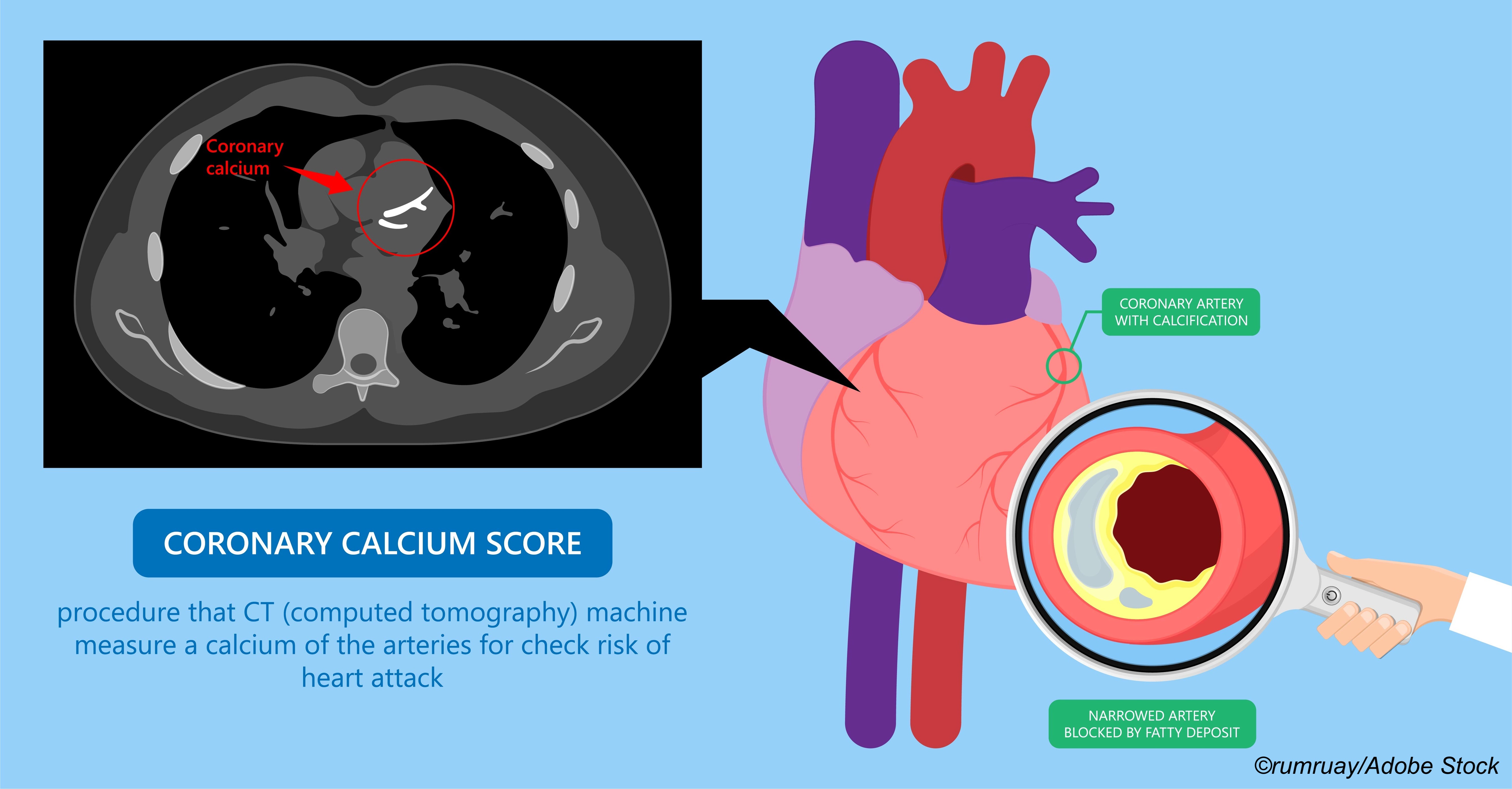
The presence of coronary artery calcium (CAC) detected and measured by imaging is a significant predictor of atherosclerotic cardiovascular disease (ASCVD) mortality, but who should be screened for CAC, and when should screening be initiated?
A modeling study by researchers led by Omar Dzaye, MD, of the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease in Baltimore, suggested that 42 is the optimal age to initiate screening for men without risk factors for ASCVD and 58 for women without ASCVD risk factors, but for persons with diabetes the optimal age to initiate CAC screening is 37 for men and 50 for women.
Using those parameters, one person with a CAC score of >0 would be detected for every 4 individuals screened. The findings were reported in the Journal of the American College of Cardiology.
Additionally, the model predicted these optimal screening ages based on other risk factors:
- Family history of CHD: Age 53 for women; 39 for men.
- Current smoker: Age 53 for women; 40 for men.
- Dyslipidemia: Age 52 for women; 39 for men.
- Hypertension: Age 53 for women; 39 for men.
- Family history of CHD + dyslipidemia: Age 48 for women; 36 for men.
- Family history of CHD + hypertension: Age 49 for women; 36 for men.
In all, about a third of “younger persons with an overall low predicted 10-year ASCVD risk had premature CAC,” they wrote.
Dzaye and colleagues said that ASCVD risk equations currently used to quantify risk use CAC thresholds of >0 or < 100 for mild coronary atherosclerotic plaque burden, with >100 representing “potential for progression toward very high CAC scores (≥1,000) reflective of secondary prevention risk. However, such approaches may have limited value in younger adults because of the strong reliance of ASCVD equations on age, and lower expected CAC burden in young adults.”
With that in mind, Dzaye and colleagues developed a model based on factors that could best inform timing of CAC screening in younger adults.
The study population—22,346 participants age 30-50—underwent non-contrast computed tomography over a 20-year period (1991-2010) at four high volume centers that comprise the CAC Consortium: Cedars-Sinai Medical Center in Los Angeles, PrevaHealth Wellness Diagnostic Center in Columbus, Ohio, Harbor UCLA Medical Center in Torrance, California, and the Minneapolis Heart Institute.
All of the participants were free of ASCVD symptoms as the time of screening but were referred for scans based on family histories or underlying risk factors.
“Participants were on average 43.5 years of age, 25% were women, 12.3% were of non-White ethnicity, and there were 7,686 young persons (34.4%) with CAC >0 ,” they wrote. “Among those with CAC >0, the median (Q1, Q3) CAC score was 20 AU (4, 78 AU), and 6,080 persons (79.1%) had prevalent CAC <100. A majority of participants (92.7%) had a low 10-year risk, whereas dyslipidemia (49.6%) and a family history of CHD (49.3%) were the most common ASCVD risk factors. In total, 1 in 5 participants had hypertension (20.1%), whereas a smaller proportion had diabetes (4.0%) or were active smokers (11.0%).”
Diabetes had the “most robust association with earlier conversion to CAC >0, with a larger magnitude effect in women (β=0.71) compared with men (β=0.63).” The authors noted that the predictive utility of CAC for ASCVD outcomes “is similar in types 1 and 2 diabetes. However, individuals with type 1 diabetes may develop CAC as young as 17 years of age; therefore, further studies in this patient population are required.”
In an editorial published with study, Tasneem Z. Naqvi, MD, MMM, of the Department of Cardiovascular Medicine, Mayo Clinic, Scottsdale, Arizona, and Tamar S. Polonsky, MD, MSCI of the Department of Medicine, University of Chicago applauded the findings for “filling an important clinical gap, providing highly actionable data that could help guide clinical decision making for ASCVD prevention.”
But they pointed out a number of limitations, including the cross-sectional design and the fact that each person had just one CAC scan so the “data on first ’conversion’ of a CAC score 0 to a CAC score >0 were derived from different study participants. Only 25% of the cohort were women, 12.3% were non-White, and the study cohort was likely of higher socioeconomic status. It is therefore unclear how generalizable the data are to the broader population of the United States or non-Western countries.”
Moreover, screening at the recommended ages “could still miss a substantial number of young women with incident MI. The Atherosclerosis Risk in Communities Surveillance study demonstrated that among adults ages 35 to 54 hospitalized with MI, the mean age among women was 48. Clinical variables such as obstetric history (preeclampsia, gestational diabetes) and conditions such as lupus or other rheumatologic diseases could prompt providers to screen even earlier. CAC develops in women with pre-eclampsia about 5 years earlier than in women without pre-eclampsia. The authors acknowledged that a 25% testing yield is somewhat arbitrary, and one could use lower cutoffs. Future study should incorporate these nontraditional but important risk factors,” Naqvi and Polonsky wrote.
BreakingMED asked Dzaye about these additional factors and in an email response he explained “in our dataset we could not delve deep into diabetes, or these other interesting variables. This should be the focus of future research.”
-
In this analysis, approximately a third of young adults at-risk for coronary heart disease have premature coronary artery calcification (CAC).
-
Based on sex-specific multivariable logistic modeling for a 25% likelihood of detecting CAC, the optimal age for a first scan is approximately 37 years for men and 50 years for women with diabetes, and 42 years for men and 58 years for women without risk factors for premature atherosclerosis.
Peggy Peck, Editor-in-Chief, BreakingMED™
The study was supported in part by a research grant from the National Institutes of Health-National Heart, Lung, and Blood Institute.
Dzaye reported no relationships relevant to the contents of this paper to disclose.
Naqvi and Polonsky reported no relationships relevant to the contents of the editorial to disclose.
Cat ID: 308
Topic ID: 74,308,730,308,914,192,925,481


