Hepatocellular carcinoma (HCC) is the fourth most prevalent cause of cancer-related death worldwide, and incidence in the US has tripled in the last four decades. Liver damage resulting from Non-Alcoholic Fatty Liver Disease (NAFLD) that leads to Non-Alcoholic Steatohepatitis (NASH) is one the leading pathways to HCC in the US and comes with complex prevention and treatment dynamics due to social customs and stigma against diabetes and obesity. We will describe the NASH pathway to HCC in this blog, and the prevention, diagnosis, and treatment options for this pathway.
In a previous blog post on HCC care considerations, we described four leading risk factors and causal pathways for the development of HCC. We provide tools and resources to help you identify HCC, ways to link patients to suitable specialists, and help with finding appropriate studies and trials for your patients.
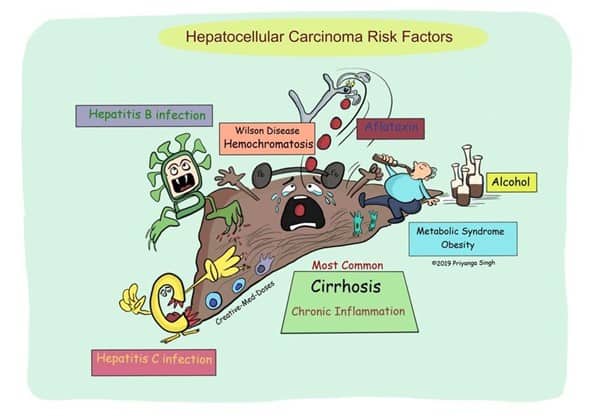
Figure 1 HCC Pathways (c) @Creativemeddose
Of the several causes of HCC shown in Figure 1, we focus on the four leading HCC risk factors:
- Hepatitis B
- Hepatitis C
- Excessive alcohol consumption
- Nonalcoholic fatty liver disease (NAFLD) leading to nonalcoholic steatohepatitis (NASH)
In this post, we focus on the NAFLD pathway to HCC.
An Emerging Health Crisis
NAFLD is an emerging collection of causes of HCC that is growing with the rise in obesity and type 2 diabetes.
An overarching social environment often exists in which food consumption is core to many social events and functions, but the food that is most available is often low quality, with high calorie count but low nutritional value. Many patients may live in areas where access to fresh produce and healthy foods is limited because of location or cost, but there is plentiful access to cheap fast food. There has been a growth in these “food deserts” in which high-energy, low-nutrition foods are cheap, available, and highly profitable while healthy foods are unavailable, poorly marketed, and require investments in kitchen equipment and skills to prepare.
NAFLD progression can be divided into four stages:
- Steatosis
Steatosis is the first and largely symptomless stage of NAFLD, and it is usually only discovered as a consequence of testing for other conditions. Steatosis was historically considered a relatively harmless condition, but evidence has accumulated that suggests this stage is neither benign nor safe to ignore. Fat deposition is a sign of incipient damage, and steatosis is already firmly on the path to HCC. - Non-alcoholic steatohepatitis (NASH)
At this stage, there is evidence of liver damage that takes the form of inflammation and apoptosis. Approximately 25% of adults in the US have NAFLD, of which approximately 20% have NASH – ~5% of US adults. At this stage, there is detectable liver damage and HCC risk is present. - Fibrosis
Persistent inflammation causes scar tissue in the liver and local blood vessels, and the damage extends in a pericellular or perisinusoidal pattern (sometimes said to be a “chicken wire” pattern). At this point, the damage is probably manifesting in ways that are observable to the patient, such as fatigue, mild upper right abdominal pain, and occasional yellowing of the skin and eyes. At this stage, the risk of HCC is elevated. - Cirrhosis
The cirrhotic liver is the final stage of damage, with often profound loss of capability and capacity, as well as overt and unmistakable health effects, including the potential for complete liver failure. Between 5% and 15% of these patients develop HCC.
NASH Risk Factors
The British NHS lists seven risk factors for NASH:
- Obesity, especially in the “apple-like” body shape
- Type 2 diabetes (often comorbid with obesity)
- High blood pressure
- High cholesterol
- Metabolic syndrome (diabetes + high blood pressure + obesity)
- Age older than 50
- Smoking
However, it must be emphasized that NASH and HCC have been diagnosed in patients who have exhibited none of these risk factors. So, while the presence of one or more should raise your index of suspicion, the absence should not be seen as ruling out NASH.
How likely are you to encounter NASH risk factors in patients?
With 25% of the US population already at the NAFLD stage, primary care physicians are likely to have a large patient population who already has NASH and can develop HCC, with approximately 5% of their patients having progressed from NAFLD to NASH. The future outlook for the NASH/HCC pathway is grim, and Markov projection models suggest a steady climb in NAFLD, NASH, and HCC.
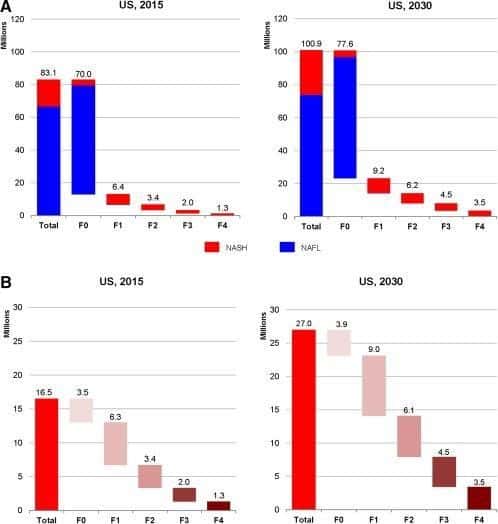
Figure 1 Distribution of the NAFLD and NASH population by fibrosis stage in the United States for 2015 and 2030. (A) NAFLD; (B) NASH. (Estes et al, 2018)
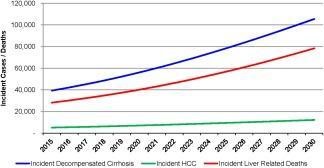
Figure 2Incident decompensated cirrhosis, HCC, and liver‐related deaths among the prevalent NAFLD population in the United States, 2015‐2030. (Estes et al, 2018)
How to discuss NASH with patients
There are many resources to assist primary care physicians in educating their at-risk patients and their caregivers. The following list provides current patient education resources (Chopra, 2020)
- Patient education: Nonalcoholic fatty liver disease (The Basics)
- Patient education: Type 2 diabetes: Overview (Beyond the Basics)
- Patient education: High cholesterol and lipids (Beyond the Basics)
- Patient education: Losing weight (Beyond the Basics)
- Patient education: Type 2 diabetes: Treatment (Beyond the Basics)
- Management of nonalcoholic fatty liver disease in adults
The American Liver Foundation provides an educational series on NAFLD. NASH, and Cirrhosis.
How to discuss HCC staging with the patient
Discussing HCC staging with patients can be difficult. The public literature available to patients often contains misleading information, while the most trustworthy and authoritative information is usually aimed at clinicians and often only available behind paywalls. Blue Faery provides clinically accurate materials that the patient will find understandable. These materials are designed to assist the physician in describing the staging and to help patients to understand where they are in the spectrum.
These materials include:
- The HCC patient education brochures, written in layman’s terms and intended for patients to read.
- The Blue Faery HCC staging discussion pad, which contains anatomical graphics and easily understood text. Each double-sided sheet has space for clinicians to add notes for their patients to use after an appointment.
- The Patient Resource Guide for Liver Cancer is a 20-page booklet with explanations and resources pertinent to patients with HCC and their caregivers.
Blue Faery will send these free materials to any requesting physician.
How to find HCC specialists, Treatment options, clinical trials
The treatment of HCC is best approached with a multidisciplinary team coordinated by a primary care physician. The most effective approach will likely require the expertise of multiple medical professionals and may include an oncologist with experience in HCC, a gastroenterologist, hepatologist, interventional radiologist, radiation oncologist, surgical oncologist, and a transplant surgeon.
To find all clinical trials, the best option is clinicaltrials.gov, but this website can be confusing and difficult to navigate. To assist clinicians in guiding patients to relevant trials, Blue Faery provides a custom HCC clinical trial navigator.
Community Support for Patients With HCC
Patient communities help provide patients with practical tips for their care journey and are often a source of emotional support by people who understand the experience.
The Blue Faery Liver Cancer Community is a free, HIPAA-compliant online community where patients and caregivers are welcome to join and to seek or exchange information relevant to HCC care. Members ask questions, discuss concerns, and find common ground as they navigate their cancer journeys. The forum moderators include community ambassadors who were former caregivers of patients with HCC.
For one-on-one patient support, Blue Faery has partnered with Imerman Angels, a nonprofit organization that provides peer-to-peer support services for the liver cancer community. Blue Faery and Imerman Angels believe that no one should face cancer alone.
Conclusion
There is a pressing need to address NASH risk factors, and combat the steady climb in obesity and Type-2 diabetes that can fuel a progression from NAFLD to NASH to HCC. To further aid in the care of those who have developed HCC, Blue Faery provides free, patient-readable, and clinically accurate materials to assist clinicians in discussing their patients’ staging, options, and resources.



 PWeekly
PWeekly