Endovascular thrombectomy (EVT) 6-24 hours after ischemic stroke onset was of similar benefit whether patients had a perfusion mismatch or clinical mismatch imaging profile, an analysis of pooled patient-level data found.
EVT was associated with an ordinal improvement in 90-day modified Rankin Scale (which ranges from 0, indicating no disability, to 5, indicating severe disability) for the clinical mismatch group (n=295; OR 3.57, 95% CI 2.29-5.57, P<0.001) and for the perfusion mismatch group (n=359; OR 1.13, 95% CI 2.10-4.66, P=0.001), compared with no EVT, reported Gregory Albers, MD, of Stanford University, and co-authors in JAMA Neurology.
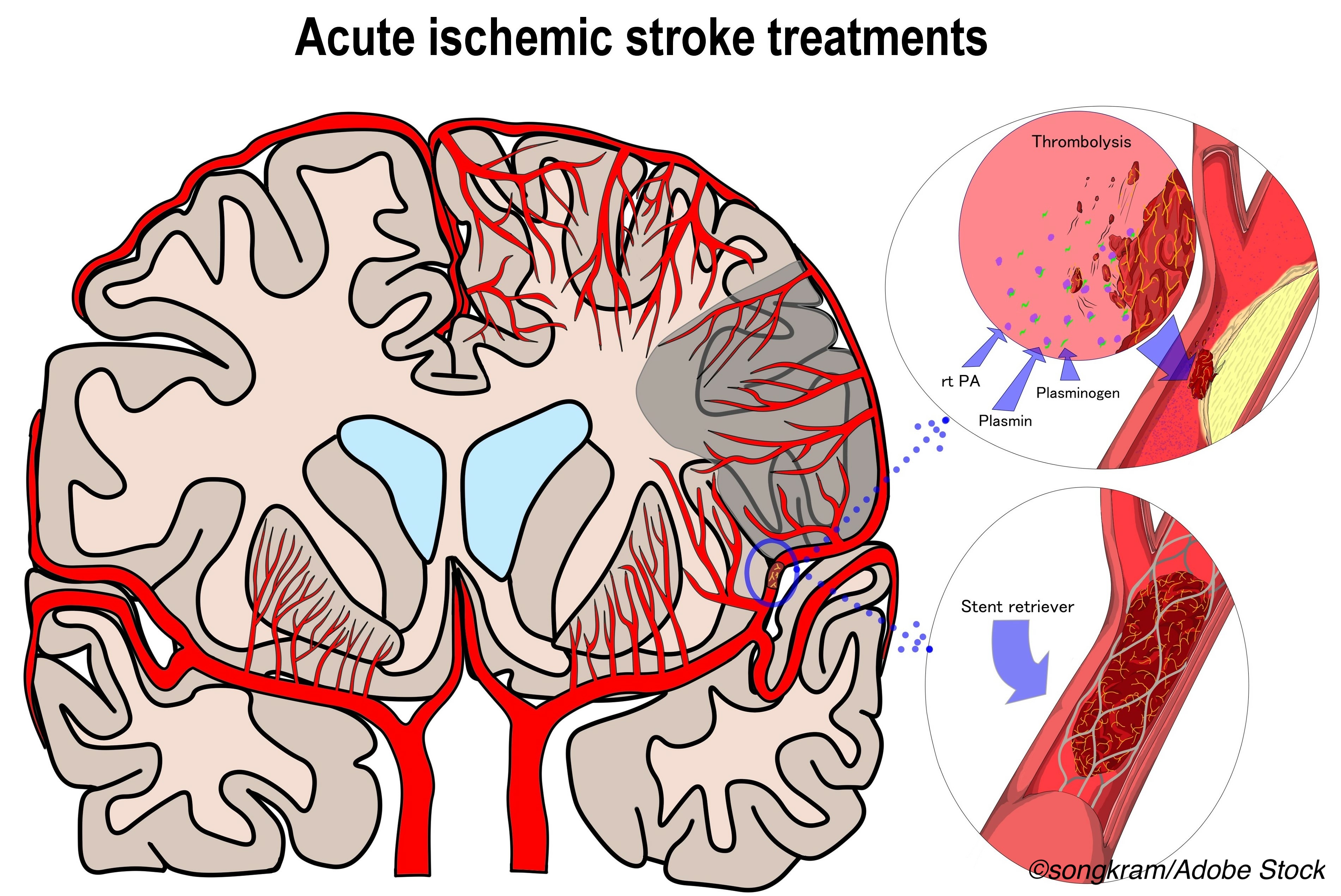
Current guidelines recommend an EVT treatment window of 6-16 hours after stroke onset for those with a perfusion mismatch and 6-24 hours for those with a clinical mismatch, but whether those with perfusion mismatch would benefit from EVT out to 24 hours has been unknown. Both forms of mismatch imply a hypoperfused penumbra of salvageable tissue surrounding a core infarct that can be saved with rapid restoration of normal perfusion.
“To our knowledge, this study provides the first data on the benefits of endovascular therapy among patients with a target perfusion mismatch profile beyond 16 hours after they were last known well,” Albers and colleagues wrote. “The associated benefits for these patients were substantial.”
“These findings support EVT as a treatment for patients meeting the criteria for either of the imaging mismatch profiles within the 6- to 24-hour interval,” they added.
The researchers analyzed pooled data from the AURORA collaboration of six randomized clinical trials that included patients (n=505) with anterior circulation ischemic stroke enrolled 6 hours or more after symptom onset who were randomized to EVT with second-generation thrombectomy devices or no EVT. Mean age was 68-69 and 53-54% were men. Mean baseline National Institutes of Health Stroke Scale score (range 0-42, with higher scores indicating more severe stroke) was 16.4 in the EVT group and 17.2 in the non-EVT group.
Data for 373 patients (74%) allowed both profiles to be determined; 96.5% met criteria for perfusion mismatch and 79.3% for clinical mismatch. For 132 patients (26%) with an undetermined imaging profile, no significant treatment benefit was seen (OR 1.59, 95% CI 0.82-3.06; P=0.17).
“Using a 24-hour interval for endovascular therapy and treatment of patients who meet either the clinical or target perfusion mismatch profile will increase the number of patients who can be treated,” the researchers noted. “In the present study, patients who had an undetermined mismatch profile because perfusion imaging was not performed did not experience a treatment benefit, and a significant interaction between treatment effect and mismatch status was found.”
“The results are clear. Thrombectomy was associated with equal benefits among patients with the two mismatch profiles,” wrote Jean-Claude Baron, MD, ScD, of Université de Paris in France, in an accompanying editorial.
“This important finding, derived from optimal randomized controlled trial data sets, suggests that the target mismatch profile (i.e., mismatch derived from perfusion imaging) can be safely applied not only in the 6- to 16-hour window but also in the 16- to 24-hour window,” he added.
Brain ischemia involves a core infarct of non-rescuable tissue with a variable penumbra of hypoperfused but potentially salvageable tissue on its periphery. If a substantial penumbra is inferred through imaging, a perfusion mismatch is identified. Similarly, a severity mismatch between clinical presentation and findings on non-perfusion CT or MRI imaging also suggests a penumbra due to clinical mismatch.
Current guidelines were based on the DAWN and DEFUSE 3 trials of EVT versus no EVT in stroke. DAWN used a 6-24 hour treatment window based on clinical mismatch and DEFUSE 3 used a 6-16 hour treatment window based on perfusion mismatch.
“However, these criteria only encompass approximately 3% of all patients with acute ischemic stroke, 6% of those presenting in the 6- to 24-hour window, and 30% of all potentially eligible patients (i.e., those presenting with large-vessel occlusion and National Institutes of Health Stroke Scale [NIHSS] scores ≥6 or within the 6- to 24-hour window) eligible for thrombectomy,” Baron observed.
The present study defined an age-based clinical mismatch profile for patients 80 years or older as a NIHSS score of 10 or higher and an ischemic core volume of less than 21 mL. For people younger than 80, clinical mismatch was either an NIHSS score of 10 or higher and an ischemic core volume of less than 31 ml or an NIHSS score of 20 or higher and an ischemic core volume of 31 to less than 51 mL.
Perfusion mismatch was defined as an ischemic core volume of less than 70 mL, a ratio of volume of critically hypoperfused tissue to ischemic core volume of 1.8 or higher, and an absolute volume of potentially reversible ischemia (estimated penumbra) of 15 mL or more.
The analysis included adjustment for age, sex, stroke severity, site of occlusion (internal carotid artery, M1 segment of the middle cerebral artery, or M2 segment of the middle cerebral artery), time from stroke onset to randomization, and other clinical data.
Limitations of the study included an underpowered analysis of the 132 patients with an unknown mismatch profile. Favorable numerical differences that were observed in functional independence at 90 days “could be clinically relevant if the analysis were adequately powered,” the researchers wrote. In addition, the study did not include patients who received treatment less than 6 hours after stroke onset.
-
Endovascular thrombectomy (EVT) 6-24 hours after ischemic stroke onset was of similar benefit whether patients had a perfusion mismatch or clinical mismatch imaging profile, an analysis of pooled patient-level data found.
-
Findings support EVT as a treatment for patients meeting the criteria for either of the imaging mismatch profiles within the 6- to 24-hour window.
Paul Smyth, MD, Contributing Writer, BreakingMED™
The AURORA collaboration was funded by a grant from Stryker Neurovascular.
Albers reported receiving consulting fees from Genentech and owning equity in iSchemaView outside the submitted work.
Baron reported no conflicts of interest.
Cat ID: 38
Topic ID: 82,38,254,730,8,38,192,925