There was a time, during my training and early in my career when the trauma surgeon was the fighter pilot of the surgical world. We were the Top Knives, the Master Surgeons, of our respective hospitals. Certainly the surgeons who trained me in the craft embodied that, and it was something I aspired to.
The nature of trauma has changed over the thirty years since I finished my residency. Penetrating trauma has fallen off to less that 15% of our total evaluations at the same time that non-operative management of liver and splenic injuries has become the norm. Cars are safer than they were 2 decades ago and the injury patterns have changed as a result.
I recently reviewed my trauma experience for the past year in preparation for applying for the ABS recertification exam.
I attended 518 Level 1 trauma activations in the past year. Of those, 294 were admitted as Trauma Service patients. Out of that total I did 21 major surgical procedures (not counting sewing up lacerations or chest tube placements in the trauma bay).
“I fear that trauma surgeons have gone from being the Master Surgeons, to the lifeguards at the shallow end of the gene pool.”
Those numbers seem to be in line with reported national averages. Operative intervention is now only a small part of what the trauma surgeon does, although I would argue that the acuity of those operative cases is higher than it was 20 years ago.
I reviewed the charts of the trauma admissions with which I was involved. 86% presented with a blood alcohol level in excess of 0.08 g/dl, or legally intoxicated. 47% returned a positive urine drug screen for other drugs such as opioids, benzodiazepines, methamphetamine, or marijuana. 76% were uninsured or underinsured (meaning that without the stop-loss portion of my trauma contract, I would not have been paid for my work).
The trauma service these days consists mainly of babysitting recovering orthopedic and neurosurgical patients. That’s not to say that these patients don’t have ongoing problems that are best managed by a team of surgeons, but they are not patients that we as trauma surgeons have operated on. All too often, the operating service signs off on day 3 or 4, and we are left doing the bulk of the postoperative care, rehab care, and discharge planning.
Not terribly exciting to a fighter pilot personality. I fear we have gone from being the Master Surgeons, to the lifeguards at the shallow end of the gene pool.
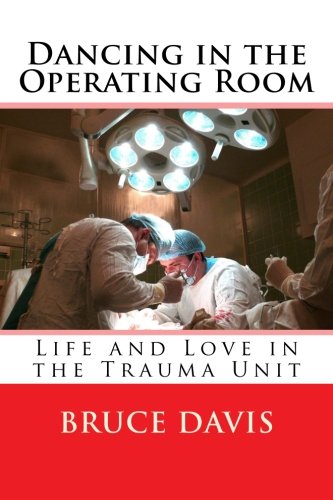
Like What You’re Reading?!
Get Dr. Davis’s new book, Dancing in the Operating Room, a collection of these and other short essays about life and love in the world of surgery and medicine, now available from Amazon in print or as an e-book. Check it out!


