Research indicates that women with early-stage endometrial cancer who have lymphovascular space invasion on their hysterectomy specimen have more aggressive tumors that are more likely to spread to the lymphatics, more likely to recur, and are associated with poor survival. However, consensus is lacking on the optimal treatment for these patients in order to prevent recurrence and improve survival, explains Anna L. Beavis, MD, MPH. “Moreover, more and more data show that a tailored, specific approach to cancer treatment optimizes outcomes,” she adds. “Not all endometrial cancers are the same, and with regard to treatment, one size may not f t all.”
Comparing Treatment Modalities
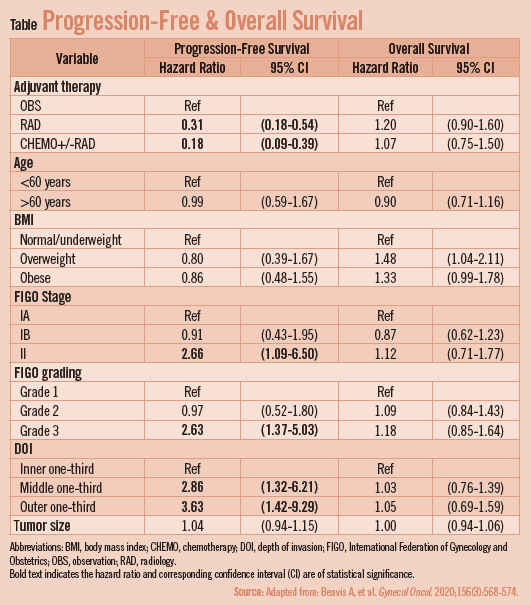
For a study published in Gynecologic Oncology, Dr. Beavis and colleagues compared progression-free and overall survival in women with stage IA-II endometrial cancer with endometrioid histology with lymphovascular space invasion who were treated with surveillance alone, radiation (external beam and/or vaginal brachytherapy) alone, or systemic chemotherapy with or without radiation. “We were particularly interested in the effect of chemotherapy on recurrence risk in this population,” notes Dr. Beavis. “We therefore formed a collaboration between eight institutions, combining data from the prospective endometrial cancer databases of each.”
All 478 participants had undergone hysterectomy with or without lymphadenectomy from 2005- 2015, had a median age of 64, and were followed for a median of 50.3 months. Following surgery, 30% underwent observation, 48.5% received radiation only, and 21.5% received chemotherapy, 95% of whom also received radiation. Although demographics were similar among the groups, those undergoing observation had lower tumor stage and cancer grade. Risk of recurrence was assessed after controlling for factors known to be associated with recurrence, including age, tumor grade, and cancer stage. “We also tested our hypothesis that chemotherapy would have a different effect on grade III tumors compared with grade I/II tumors by testing for an interaction and looking at the treatment effects in grade III tumors alone,” Dr. Beavis explains.
Improved Recurrence Rates
Overall, recurrence occurred in 21% of women. Compared with observation alone, progression-free survival was improved with both chemotherapy with or without radiation (hazard ratio [HR], 0.18) and radiation alone (HR, 0.31). “However, in the total cohort, neither radiation nor chemotherapy with or without radiation was superior to the other,” notes Dr. Beavis. “That said, when we looked specifically at grade III tumors—which are known to be more aggressive— we found that the treatment group who received chemotherapy (of whom 95% also had radiation) had lower recurrence rates compared with those who received radiation alone or surveillance. Unfortunately, overall survival did not diff er by group, regardless of grade, though we did not have the power to detect a difference in our study.”
Additional Research Needed According to Dr. Beavis, the study findings suggest a potential role for chemotherapy in the adjuvant setting for early-stage, high-grade endometrial cancer with lymphovascular space invasion. “However,” she says, “this is only hypothesisgenerating data and something that needs further study in a trial before being used to change clinical practice.” To that end, Dr. Beavis notes the need for future research focused on individualizing treatment for early-stage endometrial cancer based on tumor and molecular characteristics. “In the United States, we could consider a cooperative group trial evaluating the eff ect of chemotherapy in grade III tumors with lymphovascular space invasion, in order to better clarify the role chemotherapy may play in adjuvant therapy for early-stage endometrial cancer,” she adds.



 Janine Anthes
Janine Anthes