For several years, Medicare has tied hospital reimbursement to its definition of quality of care. Poorly performing hospitals can be penalized as much as 2% of their Medicare payments.
As part of Medicare’s assessment of quality, surveys are used to measure patient experience and satisfaction. One of the components of the Medicare survey is pain management, which Medicare describes as follows:
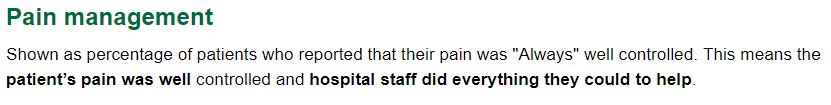
I’m not sure who, if anyone, does Medicare’s copy editing, but that’s the way it looks in a screen grab from the website. The emphasis on “always” controlling pain, which many patients equate with “no pain,” is one reason we have an opioid epidemic.
How valid is patient satisfaction as a measure of quality? Some conflicting research has been done, but a recent paper from JAMA Internal Medicine implies the answer is “probably not valid.”
Researchers from the Department of Family and Community Medicine at the University of California, Davis surveyed 1141 patients immediately after they made 1319 visits to 56 different family doctors; 897 visits involved one or more patient requests with 1441 (85%) fulfilled. The authors did not comment on that percentage, but acquiescing to 85% of patient requests seems quite high.
From 10% to 18% of patient requests for pain medication, referrals, laboratory tests, and new medications other than antibiotics or pain medication were refused and resulted in statistically significant decreases in patient satisfaction of 9 to 20 percentiles after the results were adjusted for numerous patient characteristics known to affect patient satisfaction such as age, sex, race/ethnicity, education, marital status, body mass index, overall self-rated health, mental health status, personality factors, life satisfaction, worry about symptoms, prior visits with the clinician, and my personal favorite—medical skepticism.
Refusals of patient requests for radiology tests, antibiotics, other tests, occurred in 34%, 14%, and 9.5%, respectively, but these denials did not cause significant decreases in patient satisfaction percentiles.
Antibiotics were requested only 107 times—a small sample size, which may account for the lack of association with lower patient satisfaction ratings. The authors suggested clinicians might have more experience denying antibiotic requests because of recent emphasis on this topic.
They felt that a solution to the problem of lower patient satisfaction after denial of requests could be addressed by “targeted clinician training in brief communication techniques to address patient requests.” This training could be based on creating a positive patient experience while denying inappropriate requests such as adopting what they called a “wait and see” approach when a patient asked for something that the clinician did not think was indicated. Whether patients would be satisfied with that strategy is unknown.
Another option the authors did not consider might be to educate the patients about realistic expectations and the costs associated with unnecessary care.
In my opinion an even better solution would be to abolish patient satisfaction surveys.
Skeptical Scalpel is a retired surgeon and was a surgical department chairman and residency program director for many years. He is board-certified in general surgery and a surgical sub-specialty and has re-certified in both several times. For the last 8 years, he has been blogging at SkepticalScalpel.blogspot.comand tweeting as @SkepticScalpel. His blog has had more than 3,000,000 page views, and he has over 18,000 followers on Twitter.


 SkepticalScalpel
SkepticalScalpel