A couple of recent papers highlight some issues contributing to the increasing cost of medical care.
In the 10 years from 2005 to 2015, chief executive officer compensation at 22 of the top nonprofit hospital systems rose 93% from an average of $1.6 million to $3.1 million. When compared to what orthopedic surgeons made, CEO income rose from a 3 to 1 to a 5 to 1 ratio over the same time. The differential was even higher when CEO compensation was compared to that of pediatricians and registered nurses.
Similar comparisons were true for hospital chief financial officers. The hospitals involved included such famous names as Mayo Clinic, Johns Hopkins, New York-Presbyterian, and Stanford.
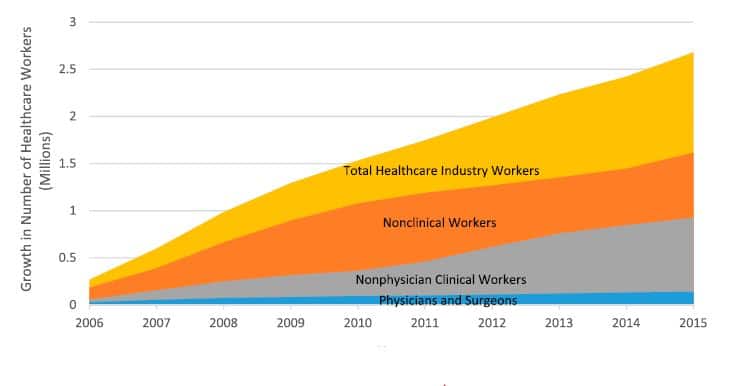
The study, from Case Western Reserve University, also found that the number of healthcare workers in the US increased by 20% from 13 to more than 15 million while the number of inpatient stays decreased by 5% over the 10-year period studied. Nonclinical workers accounted for 27% of the increase. From the paper, “In 2015, for every physician, there was 1 management worker, 10 nonclinical workers, and 14 nonphysician clinical workers.”
The figure below shows the trend over the years 2005 to 2015. Yellow is the number of total healthcare industry workers; orange indicates nonclinical workers; gray is nonphysician clinical workers; blue represents the minimal increase in the number of physicians and surgeons.
 If you are wondering what some of the nonclinical workers are doing, a paper from the Massachusetts General Hospital looked at the annual cost of its quality and patient safety program. For a single fiscal year, the total direct operating cost of the MGH quality and safety effort was almost $30 million. It was broken down as follows: QI and safety were about 39% each; measuring and reporting accounted for 19%; almost 3% was spent on training and communication.
If you are wondering what some of the nonclinical workers are doing, a paper from the Massachusetts General Hospital looked at the annual cost of its quality and patient safety program. For a single fiscal year, the total direct operating cost of the MGH quality and safety effort was almost $30 million. It was broken down as follows: QI and safety were about 39% each; measuring and reporting accounted for 19%; almost 3% was spent on training and communication.
Over $24.5 million (81%) of the money went for “regulatory or reporting requirements mandated by The Joint Commission, CMS, the state department of public health” and other such organizations. The hospital had a staff of 180.6 FTEs working on quality and safety. Their salaries made up about 90% of the direct costs of the program.
The nearly $30 million figure did not include indirect costs of overhead estimated at 3.5 to $4.5 million.
Although what goes on at MGH cannot necessarily be extrapolated to all hospitals, the authors estimated that US hospitals probably spent at least $17.2 billion per year for quality and safety programs.
Ironically, this paper appeared in The Joint Commission Journal on Quality and Patient Safety. The Joint Commission, the group that helped create opioid epidemic, was the subject of a recent BMJ paper which found hospitals accredited by TJC essentially had no better outcomes in mortality or readmission rates for 15 common medical conditions than hospitals accredited by state or independent accrediting bodies.
But don’t worry. The Joint Commission’s net assets at the end of calendar year 2017 were $276,684,688.
Skeptical Scalpel is a retired surgeon and was a surgical department chairman and residency program director for many years. He is board-certified in general surgery and a surgical sub-specialty and has re-certified in both several times. For the last 8 years, he has been blogging at SkepticalScalpel.blogspot.com and tweeting as @SkepticScalpel. His blog has had more than 3,000,000 page views, and he has over 18,000 followers on Twitter.



 Janine Anthes
Janine Anthes