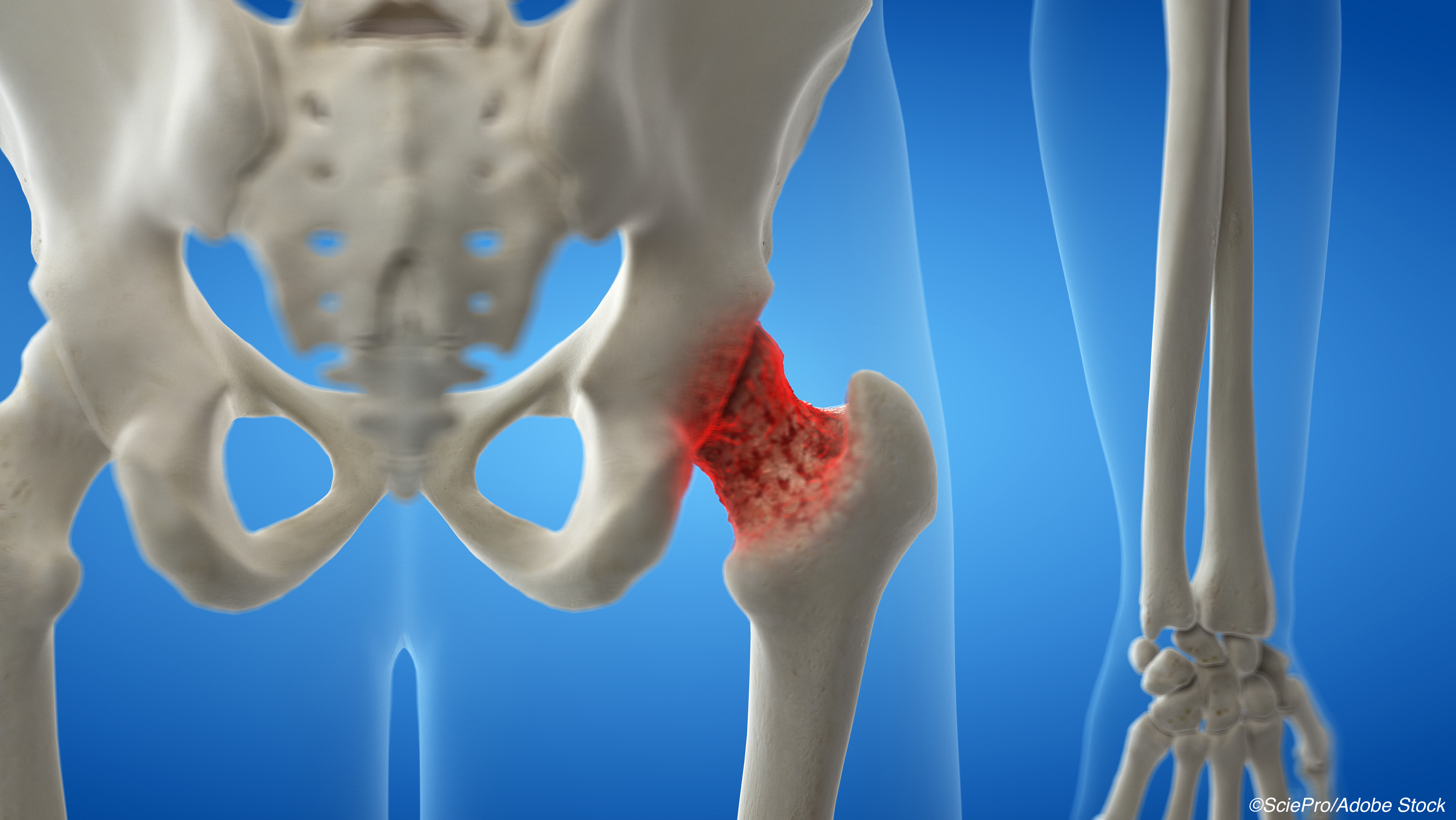
A drug holiday from osteoporosis medications may be on deck for many patients and their physicians, but taking a break from one bisphosphonate was tied to a modest bump in hip fracture risk, researchers reported.
In a study that compared the risks of drug holidays after long-term (≥3 years) of risedronate (Actonel, Atelvia) versus alendronate (Binosto, Fosamax Plus D, Fosamax), hip fracture rates were higher with drug holidays from the former bisphosphonate versus the latter at 12.4/1,000 patient years (PY) and 10.6/1,000 PY events, respectively (hazard ratio 1.18, 95% CI 1.04 to 1.34) for a total of 915 hip fractures in the studied time period (November 2000 and March 2020), according to Kaleen N. Hayes, PharmD, PhD, of the Brown University School of Public Health in Providence, Rhode Island, and co-authors.
They also reported in the Annals of Internal Medicine that the association was attenuated with:
- Any fracture included as the outcome: HR 1.07 (95% CI 1.00 to 1.16).
- Shorter drug holidays: HR 1.03 for 1 year [95% CI 0.85 to 1.24); HR 1.14 for 2 years (95% CI 0.96 to 1.32).
Hayes and co-authors noted that, yes, they found “an 18% increased relative risk for hip fracture over 3 years,” but also explained that “[t]his relative effect reflects a low increased absolute risk (3-year risk difference of 0.6 percentage points), with a corresponding number needed to treat of 167 patients with alendronate instead of risedronate to prevent one hip fracture.”
In general, drug holidays have proven to be a fractious topic in the musculoskeletal health community. A study presented at the 2017 American College of Rheumatology meeting demonstrated that women who stopped using bisphosphonates for more than 2 years faced a significantly higher risk of a hip fracture versus those who continued treatment. At the time, study author Jeffrey Curtis, MD, MS, MPH, of the University of Alabama at Birmingham, noted in a press release that “the notion of a drug holiday has become commonplace in osteoporosis management,” but that “there’s a dearth of evidence on when we should consider restarting bisphosphonate therapy.” The results from Curtis’ group held firm in a 2020 Medical Care study.
Several studies — FLEX, HORIZON, VERT-NA, and FIT — bolstered the concept of osteoporosis drug holidays. However, a 2011 FDA panel reviewed the long-term safety and efficacy of bisphosphonates and voted that “labeling for these drugs should further clarify the duration of use for bisphosphonates but there was a lack of panel consensus on label changes. The FDA wrote their opinion on this perspective, suggesting reevaluation of the need for continuing bisphosphonate therapy beyond 3-5 years in individual patients. The FDA suggested that a drug holiday may not be advisable in high-risk patients, but for patients discontinuing treatment, there were no concrete recommendations on what should be done,” noted Dima L. Diab, MD, of the Cincinnati VA Medical Center, and Nelson B. Watts, MD, of Mercy Health Osteoporosis and Bone Health Services in Cincinnati, in Therapeutic Advances in Musculoskeletal Disease.
Hayes and co-authors conducted a population-based, matched, cohort study using data from one Canadian province and ultimately settled on a total of 25,077 propensity score-matched pairs (mean age 81; 81% women; mean of about 6 years of therapy pre-drug holiday; 55% on risedronate; almost a quarter with a diabetes comorbidity).
In a secondary analysis, they reported sex-stratified hip fracture rates of 8.2 events/1,000 PY for men and 12.2 events/1,000 PY for women. The sex-stratified regression results were an HR 1.37 (95% CI 0.95 to 1.97) for men and HR 1.15 (95% CI 1.01 to 1.33) for women.
The authors explained that the findings “indicate that the higher hip fracture risk associated with risedronate use had an onset approximately 2 years into the drug holiday and not before. These results suggest that risedronate drug holidays may pose similar risk to alendronate drug holidays for most patients up to 2 years for hip fracture and throughout the drug holiday for all types of fractures.”
But they cautioned that they were not advocating that alendronate was superior to risedronate, and that “the decision to initiate alendronate or risedronate therapy is driven by the prescriber and may be influenced by many patient-specific considerations. For example, only risedronate is available as a monthly dosing option or a weekly delayed-release formula that does not require a fasting state like other formulations. Thus, risedronate therapy may be preferable for patients who highly value these treatment factors.”
Study limitations included the fact that Hayes’ group used healthcare administrative data that did not contain information on certain fracture risk factors, such as race/ethnicity, and that the data came from an older, 70% White population. They stated that “absolute hip fracture risk is lower among younger and non-White populations.”
So who is eligible for a drug holiday from their osteoporosis meds? In a 2021 Journal of Clinical Medicine review, Hayes’ group advised that “a drug holiday of one year may be more appropriate in patients with less total bisphosphonate exposure (e.g., three years of oral bisphosphonate treatment at low adherence, similar to 1.5 years of total exposure) due to lower residual bisphosphonate protection,” although they conceded that “robust studies examining the effects of adherence and total cumulative bisphosphonate exposure are lacking.”
In a 2020 ACR Convergence Today article, Karen Hansen, MD, MS, of the University of Wisconsin-Madison, pointed out that the decision to do a drug holiday is an opportunity for shared decision-making. Hansen explained that she’ll discuss multiple issues with the patient, such as the trajectory of bone density stability, the current T-score in the hip, and how the patient plans to maintain good bone health if they go off the medication. “In other words, not drinking too much, not smoking, continuing on with adequate calcium and vitamin D supplements, continuing on with regular exercises that are good for bone health,” she stated.
And drug holidays may not be a great idea with other osteoporosis drugs. A 2019 systematic review in the Annals of Internal Medicine showed that, after 3 to 5 years of treatment, bisphosphonate continuation versus discontinuation cut radiographic vertebral fractures, particularly with zoledronic acid, and clinical vertebral fractures with alendronate, but did not reduce the risk for non-vertebral fractures. However, the strength of the evidence was low, according to Howard A. Fink, MD, MPH, and co-authors.
In a 2021 YouTubeinterview, Janet Rubin, MD, of the University of North Carolina at Chapel Hill, told Margaret Martin, PT, of MelioGuide Physiotherapy in Ottawa, Ontario, Canada, that for the injectable monoclonal antibody denosumab (Xgeva, Prolia) “when we decide to put you [a patient] on Prolia, that’s it for you; you are staying on this drug…they are protected [when they are on denosumab] but they are at a higher risk for fractures when you stop denosumab, period. We all know that…and we’ve known that for a bunch of years now…we would just never stop denosumab.”
Hansen also stressed that drug holidays are a non-starter for patients on denosumab, teriparatide (Forteo), abaloparatide (Tymlos), and romosozumab (Evenity). “We know that the gains in bone density will be lost,” she said. “When we stop denosumab, not only are gains in bone density quickly lost, but even worse is that patients can have a rebound increase in bone breakdown and experience multiple painful compression fractures during that phase.”
Finally, Diab and Watts recommended using the 10-year FRAX risk assessment tool to “guide treatment decisions. A recent study…suggested that the FRAX tool can be used to predict fracture probability in women currently or previously treated for osteoporosis, which may help in guiding the need for continued treatment or treatment withdrawal.”
-
Osteoporosis drug holidays after long-term therapy with risedronate were linked with a small increase in risk for hip fracture versus alendronate drug holidays.
-
The absolute increased risk in the study was with a 3-year risk difference of 0.6 percentage points and a number needed to treat of 167 patients with alendronate instead of risedronate to prevent one hip fracture.
Shalmali Pal, Contributing Writer, BreakingMED™
The study was funded by the Canadian Institutes of Health Research (CIHR).
Hayes reported support from CIHR/University of Toronto (U of T), CIHR Drug Safety and Effectiveness Cross-disciplinary Training Program/U of T, and the Ontario Drug Policy Research Network Training Program/U of T. Co-authors reported relationship with, and/or support from, Amgen, Osteoporosis Canada, American Society for Bone and Mineral Research, International Society for Clinical Densitometry Canadian Panel, and the Endocrine Society.
Cat ID: 15
Topic ID: 76,15,438,730,15,187,191,142,192,925


