The addition of isatuximab (Isa), an anti-CD38 monoclonal antibody, to carfilzomib and dexamethasone (Kd) improved progression-free survival (PFS) and depth of response in patients with relapsed multiple myeloma (MM) and renal impairment (RI), an interim analysis of the phase III IKEMA study found.
In a subgroup analysis involving 61 patients with RI, defined as an estimated glomerular filtration rate (eGFR) of <60 mL/min/1.73 m2, the addition of Isa to Kd prolonged PFS by 73% (hazard ratio [HR], 0.27; 95% CI, 0.11-0.66) compared with Kd alone, Marcelo Capra, MD, Hospital Mae de Deus, Porto Alegre, Brazil, and multi-center colleagues reported in Haematologica.
The same triplet increased the proportion of patients who achieved both a complete renal response (52% versus 30.8% for those treated with the doublet) as well as a durable renal response lasting 60 days or longer (32% versus 7.7%, respectively).
A complete renal response was defined as an increase in eGFR from <50 mL/min/1.73 m2 at baseline to ≥60 mL/min/1.73 m2 one month or more later.
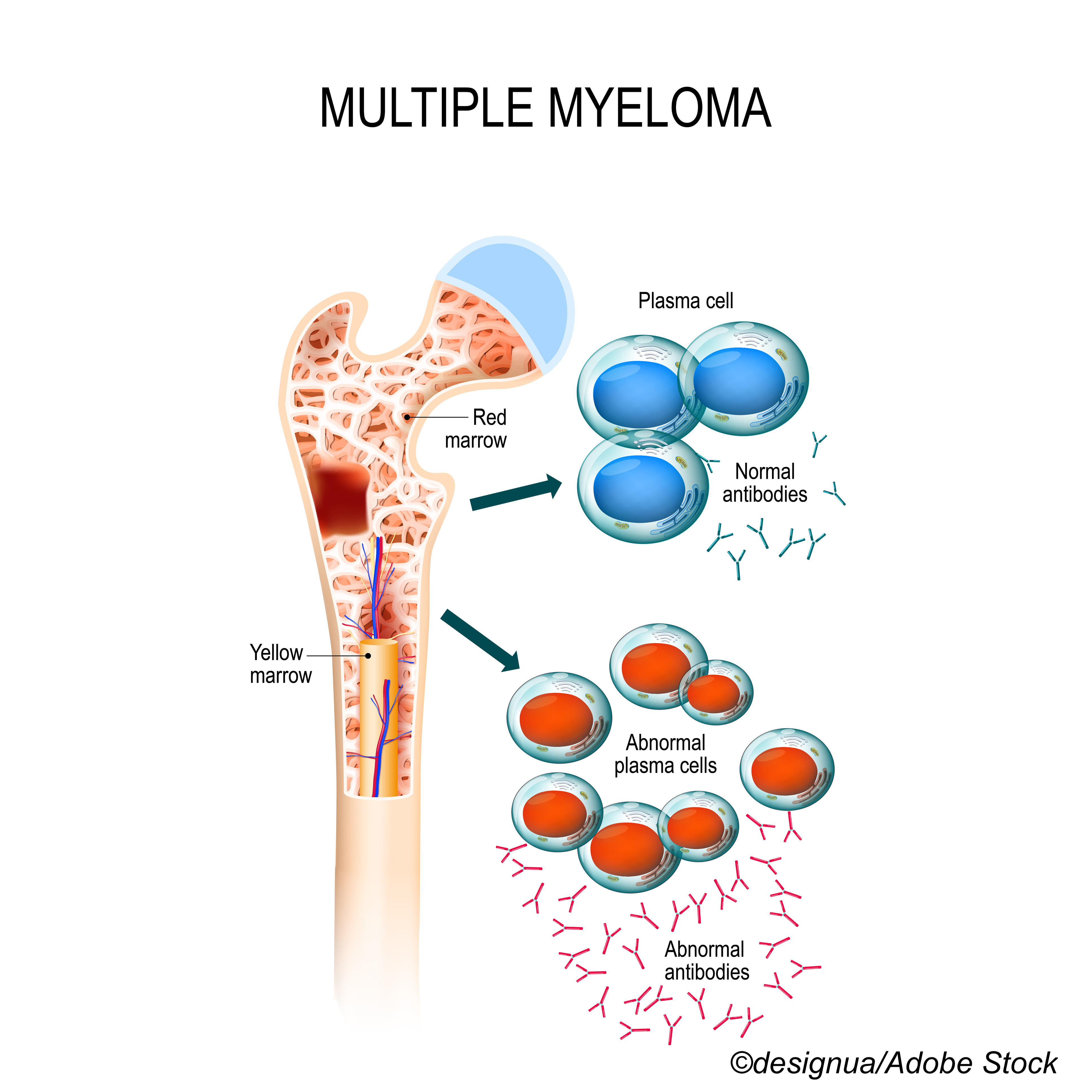
“In MM patients, RI is considered a poor prognostic factor, being associated with earlier mortality and worse OS [overall survival]. As such, there is a critical need for anti-MM therapies that also improve renal function,” Capra and colleagues observed. Renal impairment affects up to 50% of patients with MM.
“Based on [our] findings, Isa-Kd represents a valuable addition to the therapies used to treat patients with MM-related renal dysfunction,” the authors concluded.
IKEMA was a prospective, multinational, randomized, open-label study carried out at 69 study centers in 16 countries. Patients with relapsed MM who had received one to three prior lines of therapy were eligible for study enrolment, including patients with a baseline eGFR as low as 15 mL/min/1.73 m2.
Patients randomized to Isa-Kd received Isa intravenously at a dose of 10 mg/kg on days 1, 8, 15, and 22 in the first 28-day cycle and on days 1 and 15 in subsequent cycles.
In both arms, carfilzomib, a next-generation proteasome inhibitor, was also given intravenously at a dose of 20 mg/m2 on days 1 and 2; 56 mg/m2 on days 8, 9, 15 and 16 of cycle 1; and then at the same dose on days 1, 2, 8, 9, 15, and 16 of each subsequent cycle. Dexamethasone in turn was dosed at 20 mg and given orally on days 1, 2, 8, 9, 15, 16, 22, and 23. Treatment was continued until disease progression or unacceptable toxicity.
The median number of cycles for patients treated with Isa-Kd was 20 compared with a median of only 9 cycles for those treated with Kd.
The primary efficacy endpoint was PFS, investigators noted.
“At a median overall follow-up of 20.7 months, the PFS benefit of Isa-Kd versus Kd in patients with and without RI… was consistent with that seen for the overall IKEMA study population,” the authors reported.
Median PFS was not reached among renally-impaired patients treated with Isa-Kd compared with 13.4 months for those treated with Kd alone, while the likelihood that renally-impaired patients would be free of a PFS event at 18 months was 79% compared with 41% for patients given Kd alone.
“Consistent treatment effect was also observed in patients with the most severe RI at baseline,” Capra and colleagues pointed out.
Among those with a baseline eGFR <45 mL/min/1.73 m2, median PFS was again not reached for those treated with additional Isa compared with a median of 11.1 months for Kd patients.
The overall response rate (ORR) wasconsiderably higher with Isa-Kd for RI patients at 93.1% compared with 61.1% for Kd alone patients, while a very good partial response was similarly higher at 79.1% for Isa-Kd patients compared with 44.4% for Kd alone patients.
In addition, complete responses (CRs) were achieved in almost twice as many RI patients treated with Isa-Kd at 41.9% compared with 22.2% for Kd alone patients.
Looking more closely at renal responses, the time to first renal response and the time to a complete renal response were both more rapid in patients with an eGFR <50 mL/min/1.73 m2 treated with Isa-Kd compared with Kd alone.
For example, the median time to first renal response was 1.5 months (95% CI, 0.82-not calculable) in the triplet arm versus 6.5 months (95% CI, 0.69-not calculable) in the doublet arm. Median time to complete renal response was similarly shorter at 7.8 months (95% CI, 1.22-not calculable) for the Isa-Kd arm versus not calculable (1.28-not calculable) months in the Kd alone arm.
Urgent therapy is required to achieve reversal of severe RI, the authors noted, since renal failure that lasts longer than 2 weeks can substantially compromise the possibility of recovery.
Rates of grade 3 and higher treatment-emergent adverse events (TEAEs) were remarkably similar between the two treatment arms at 79.1% of Isa-Kd patients versus 77.8% of Kd alone patients. Rates of serious TEAEs were again similar between the two groups at 62.8% among Isa-Kd patients compared with 77.8% of Kd alone patients.
The most common TEAEs were diarrhea, upper respiratory tract infection, hypertension, and fatigue, rates of which were all higher in the Isa-Kd arm than in the Kd arm.
The most common hematologic toxicities in RI patients were anemia, which occurred in all patients in both arms, and thrombocytopenia, rates of which were similarly high at 93% and 83.3% for Isa-Kd and Kd, respectively.
Despite high rates of TEAEs, the authors deemed the safety profile of the triplet “manageable.”
As they also pointed out, carfilzomib has been associated with cardiac complications, and cardiac toxicity was observed in this interim analysis of patients with RI, although rates of grade 3 and higher cardiac failure were low in both treatment arms.
“More patients treated with Isa-Kd showed reversal of RI and durable renal responses compared with those treated with Kd,” Capra and colleagues concluded.
Disclosure:
The IKEMA study was funded by Sanofi.
Capra reported receiving speaker’s fees from Amgen, Janssen, and Sanofi.
by
Pam Harrison, Contributing Writer, BreakingMED™
Kaiser Health News
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation, which is not affiliated with Kaiser Permanente.

