1. Among symptomatic patients with high low-density lipoprotein cholesterol levels considered high risk for atherosclerotic cardiovascular disease (ASCVD), absence of calcified and noncalcified coronary plaque was associated with very low ASCVD event rates.
2. These results highlight the multifactorial nature of atherosclerotic cardiovascular disease being not only driven by low-density lipoprotein cholesterol levels, despite their causal pathophysiological role.
Evidence Rating Level: 2 (Good)
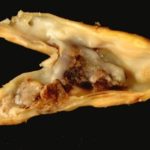
Study Rundown: Levels of low-density lipoprotein cholesterol (LDL-C) and coronary artery calcium (CAC) are frequent parameters used to assess atherosclerosis burden associated with the risk for atherosclerotic cardiovascular disease (ASCVD) events. Recent preliminary findings have suggested that some individuals with high LDL-C are resilient to developing calcified coronary plaque, as identified by a CAC score of 0. Despite this, there are concerns regarding the prevalence of noncalcified plaque in individuals with severe dyslipidemias despite a CAC score of 0. This study determined the prevalence of noncalcified and calcified plaque in symptomatic adults undergoing coronary computed tomographic angiography (CCTA) evaluation and assessed its association with ASCVD events (myocardial infarction and stroke) and death across the LDL-C spectrum. Among 23,143 symptomatic patients, absence of CAC and noncalcified plaque was prevalent in individuals with severely elevated LDL-C levels. Across the LDL-C spectrum, absence of CAC was associated with low rates of ASCVD and death, with higher rates in patients with greater CAC burden. These results highlight the multifactorial nature of ASCVD as it is not only driven by LDL-C levels, despite their causal pathophysiological role. A limitation of this study was that only symptomatic patients were included in the analysis, thus, the reported frequency of plaque and associated ASCVD events may be overstated and not representative of the asymptomatic population undergoing primary prevention.
Click to read the study in JAMA Network Open
Click to read an accompanying editorial in JAMA Network Open
In-Depth [retrospective cohort]: This cohort study included 23,143 symptomatic patients (median age [IQR], 58 [50-65] years; 12,857 [55.6%] women) undergoing CCTA between 2008 to 2017 from the Western Denmark Heart Registry. The study evaluated the prevalence of calcified and noncalcified plaque across LDL-C categories of <77, 77-112, 113-154, 155-189, and ≥190 mg/dL, where the severity of coronary artery disease was assessed via CAC scores (higher numbers indicate greater CAC burden). Overall, 1,029 ASCVD and death events occurred during a median follow-up of 4.2 years. Across the LDL-C spectrum, absence of CAC was prevalent, ranging from 46.2% in ≥190 mg/dL cohort to 54.9% in 77-112 mg/dL cohort and associated with no detectable plaque in most patients, ranging from 77.2% in ≥190 mg/dL cohort to 88.6% in <77mg/dL cohort. Across all LDL-C categories, absence of CAC was associated with low rates of ASCVD and death (6.3 [95%CI, 5.6-7.0] per 1000 person-years), with higher rates in patients with CAC scores of 1 to 99 (11.1 [95%CI, 10.0-12.5] per 1000 person-years) and ≥100 (21.9 [95%CI, 19.9-24.4] per 1000 person-years). Among those with CAC scores of 0, the event rate per 1000 person-years was 6.3 (95%CI, 5.6-7.0) in the overall population compared to 6.9 (95%CI, 4.0-11.9) in those with LDL-C ≥190 mg/dL. Across the LDL-C spectrum, rates were similar and low in those with CAC scores of 0, regardless of plaque characteristics.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.