Surgery should be the go-to treatment for acute appendicitis, although management with antibiotics-only is not out of the question for a good number of adult patients, experts stated in a review.
“Appendectomy remains first-line therapy for acute appendicitis (AA), but treatment with antibiotics rather than surgery is appropriate in selected patients with uncomplicated appendicitis,” according to Theodore N. Pappas, MD, of the Duke University Medical Center in Durham, North Carolina, and co-authors.
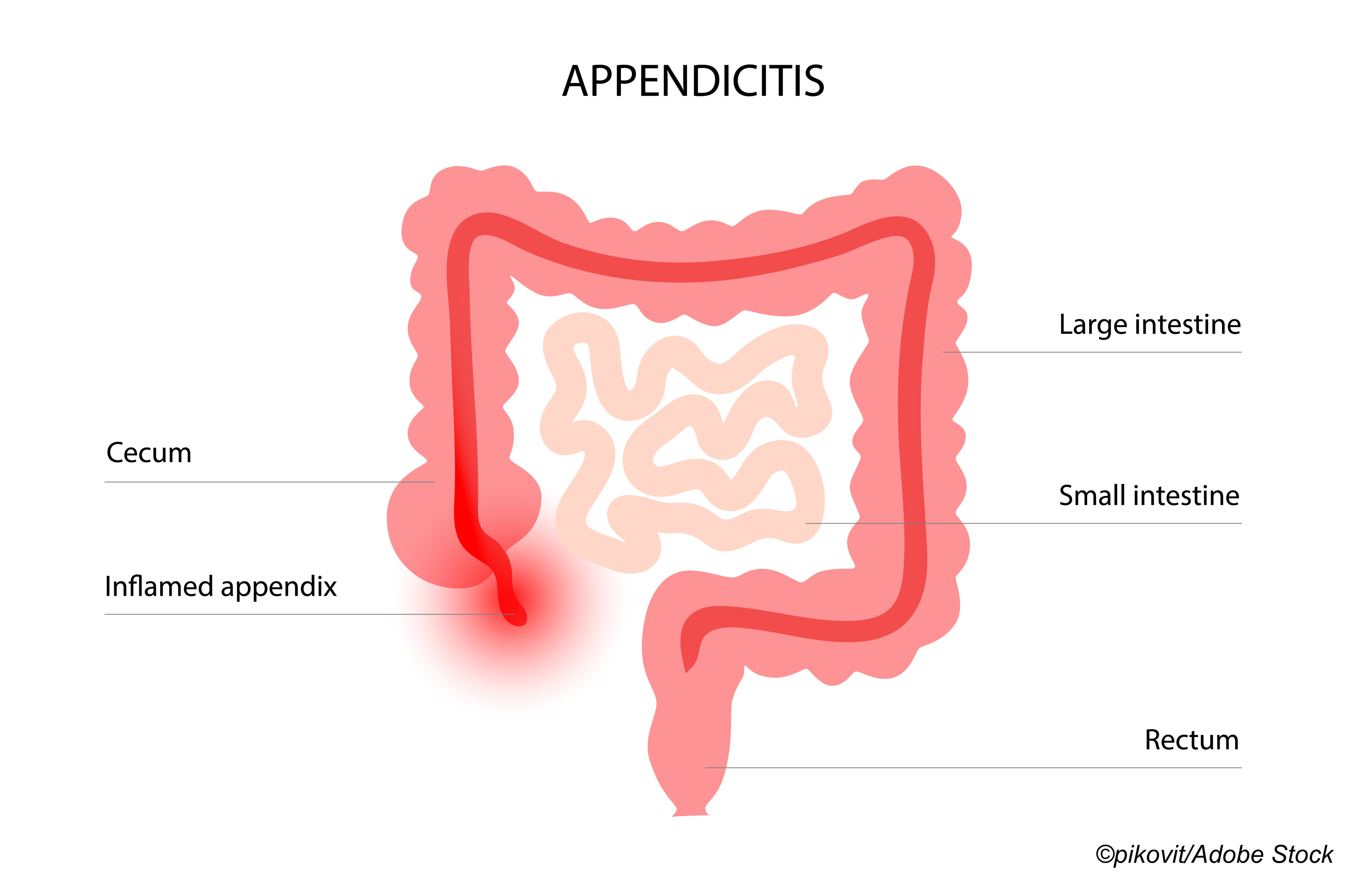
Their review “summarizes current evidence regarding diagnosis and management of acute appendicitis in adults,” they wrote in JAMA. Ultimately, they evaluated 71 pieces of published data, including 11 clinical trials, 30 observational longitudinal studies, 10 systematic reviews, nine meta-analyses, and 11 practice guidelines for the condition. As the authors noted, [a]cute appendicitis is the most common abdominal surgical emergency in the world, with an annual incidence of 96.5 to 100 cases per 100,000 adults.”
Overall, the authors recommended the following:
- In suspected appendicitis with atypical findings, “an antibiotic trial or, in very mild cases, clinical observation alone is appropriate.”
- In acute uncomplicated appendicitis, fitness for surgery should be assessed, specifically pre-operative evaluation to “estimate the risk of adverse outcomes, including the predicted postoperative morbidity and mortality.”
- In AA requiring emergency or urgent operation, pre-op “evaluation should assess the trade-off between the procedure risk and preserving long-term health.” This assessment is “usually straightforward” in younger, healthy patients.
- If the appendix is perforated and there is generalized peritonitis, pre-op “resuscitation and emergent surgical exploration are required, since these patients are typically significantly ill and may be hemodynamically unstable.”
- In clinically stable perforated appendicitis without acute illness, “the mainstay of treatment includes antibiotics with percutaneous drainage of drainable abscesses… in patients with appendiceal perforation that improves with antibiotics, reassessment and appendectomy can be considered in 6 to 8 weeks.”
- In older patients with multiple comorbidities, their level of frailty (“a lack of physiologic resilience and reserve capacity”) needs to be assessed pre-op to determine their “vulnerability to adverse events.” In patients ages >40, colonoscopy should be done to exclude cecal mass as a cause of AA.
- In appendicoliths that obstruct the appendiceal lumen and create a closed-space infection, an upfront antibiotics management approach may fail as “[in the presence of ischemia], antibiotics may be unable to effectively inhibit the inflammatory and infectious processes.”
The authors cautioned that the reviewed data only apply to adult patients and should not be generalized to children. And their proposed algorithms for AA management “have not been validated in randomized clinical trials and may not improve clinical outcomes.”
Finally, “the benefits and risks of all treatment options should be presented and discussed, and recommendations on surgery versus an antibiotics-first approach should be made based on individual clinical and radiographic findings as well as patient treatment expectations and preferences,” according to Pappas and co-authors.
The upfront antibiotics approach received a major boost from the CODA trial, which showed that non-operative treatment of appendicitis was non-inferior to appendectomy. But long-term results from the CODA trial found that at four years out, nearly half of the patients in the antibiotic study-arm ended up having an appendectomy.
Still, CODA results are meaningful for ED physicians, noted ACEP Now medical editor-in-chief Jeremy Samuel Faust, MD. A “unique aspect of CODA was that if antibiotic-treated patients met the usual discharge criteria following administration of long-acting parenteral antibiotic regimen, they could be discharged home from the [ED] and have outpatient management with completion of oral antibiotics over the next nine days,” he told ACEP Now.
Faust cited a 2017 pilot study in which >90% of antibiotic-treated patients had ED discharge, and all patients resolved the acute episode of appendicitis, versus the CODA trial where about 50% had ED discharge. “Sites varied a lot with regard to the rate of ED discharge, from never doing it to more than 80% going home at some hospitals. This may have reflected physician comfort and experience with antibiotic treatment,” he stated.
In an American College of Surgeons interview, CODA co-investigator David R. Flum, MD, MPH, of the University of Washington in Seattle, addressed the issue of appendectomy despite initial success with antibiotics in the ED.
“There are a lot of reasons why some people might wind up having an appendectomy after they make it through an initial course of antibiotics,” he stated. “There’s the risk of recurrence, and we’ve always known that was a risk…there’s also some patients who may choose to get their appendix out because they have a lot of anxiety about their appendix, or they’ve read about risks of a neoplasm… some of these appendectomy procedures may have been for reasons that…might be not be considered clinical. But altogether… we do have a better picture now of what it’s like for people after they get through the initial episode of being managed with antibiotics.”
Flum added that “about half [of patients] can avoid appendectomy [and] half will end up getting an appendectomy. I think different people—surgeons, [emergency department] doctors, patients, families—are going to view that 50-50 statistic from their own lens, and that is the beauty of the CODA trial.”
Findings from the APPAC II trial demonstrated that antibiotic monotherapy for 7 days straight led to treatment success rates of over 65% in adults with uncomplicated acute appendicitis, although this regimen failed to achieve non-inferiority versus a course of IV antibiotics followed by oral drugs. And in a related study, children who received a delayed diagnosis of appendicitis usually presented with milder symptoms, did not undergo imaging, and had worse outcomes.
Guidelines for managing appendicitis can be had from multiple groups, such as the American College of Emergency Physicians, the American Academy of Family Physicians, and the Eastern Association for the Surgery of Trauma.
In 2020, the World Society of Emergency Surgery updated its “Jerusalem” guidelines for the diagnosis and treatment of AA. The guideline states that uncomplicated AA can be treated with an antibiotics-first approach, but also warned that the “success of the non-operative approach requires careful patient selection and exclusion of patients with gangrenous AA, abscesses, and diffuse peritonitis.”
-
Appendectomy should be first-line therapy for acute appendicitis (AA), but treatment with antibiotics instead of surgery is appropriate in selected patients with uncomplicated appendicitis.
-
The recommendation is based on a review of published data and only applies to adult patients, while the proposed algorithms for AA management have not been validated in randomized clinical trials.
Shalmali Pal, Contributing Writer, BreakingMED™
Pappas reported a relationship with Transenterix.
Cat ID: 254
Topic ID: 253,254,254,730,188,192,925,159