Measurements of left ventricular end-systolic volume index (LVESVi) and volume-derived left ventricular ejection fraction (Vol-LVEF) are as effective as linear LV end-systolic dimension index (LVESDi) and linear LV ejection fraction (LVEF) in differentiating patients with hemodynamically significant aortic regurgitation (AR) who may have an excess risk of death, according to a recent study.
In addition, an LVESVi threshold of ≥45 mL/m2 was significantly associated with increased risks of mortality, the study authors reported in JAMA Cardiology.
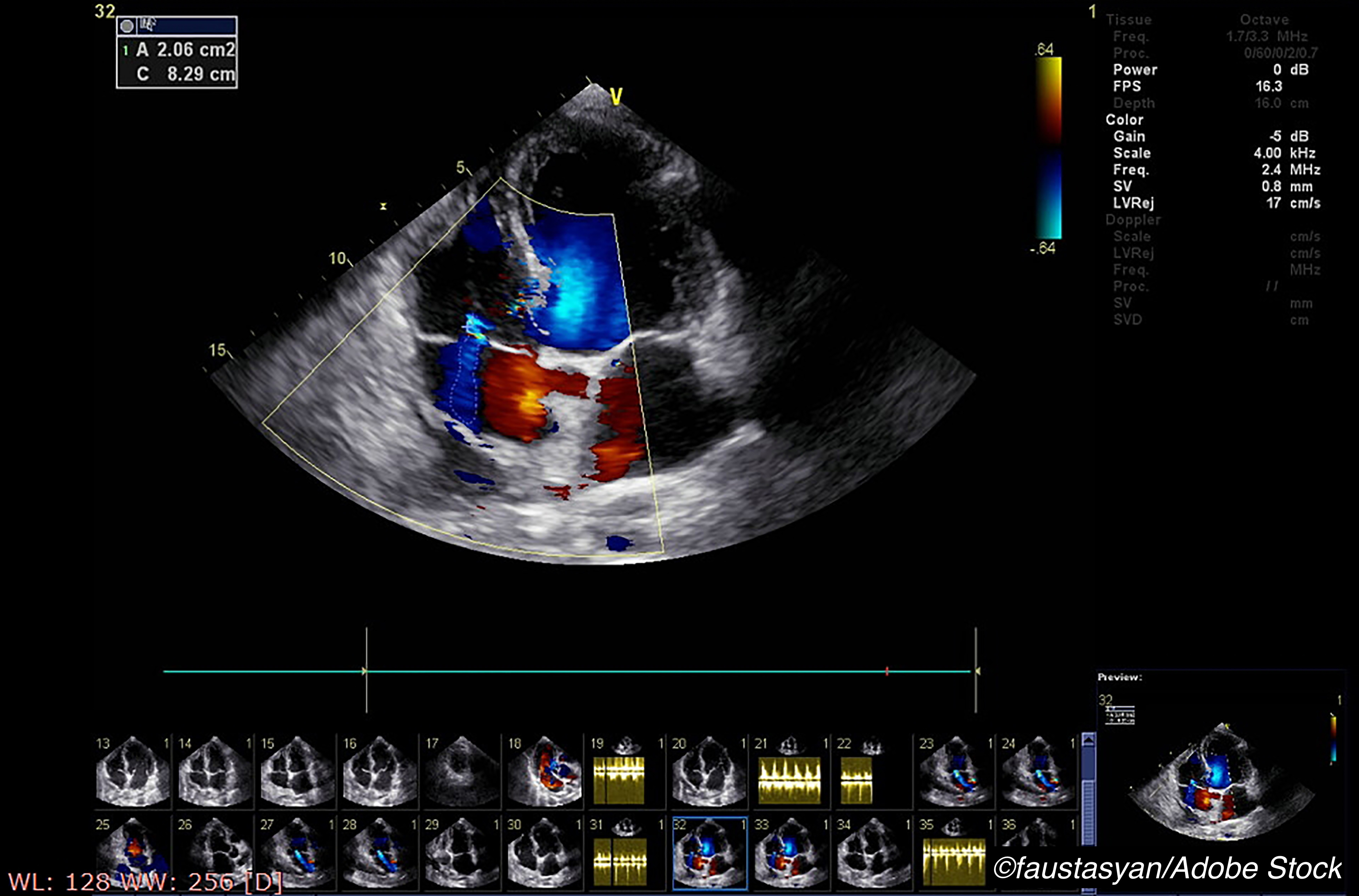
“Assessment of left ventricular (LV) function is critical for clinical decision-making in patients with valvular heart disease. Patients with hemodynamically significant AR incur excess mortality. Transthoracic echocardiography (TTE) — derived prognostic indexes in AR are based on LV linear measurements, including ejection fraction (linear LVEF), and LVESDi from studies conducted more than 2 decades ago,” explained Li-Tan Yang, MD, of the Mayo Clinic, Rochester, Minnesota, and colleagues.
“Patients with AR may remain asymptomatic for years, but when symptoms or reduced LVEF (class I indications) develop, post-AVS outcome is worse than those having surgery for non–class I indications. Therefore, it is crucial to investigate determinants of death in asymptomatic patients, and although artificial, identify thresholds for surgical timing in patients not yet attaining class I surgical indications,” they added.
Thus, Yang and colleagues conducted this study to assess whether LV volumes and Vol-LVEF can help determine mortality in patients with AR. They included 492 consecutive asymptomatic patients (mean age: 60 years; 86% male; preserved linear LVEF ≥50%; mean LVESDi: 41 mL/m2) with chronic moderately severe to severe AR, in whom they analyzed clinical and echocardiographic data and graded AR severity. LV volumes and Vol-LVEF were derived using de novo disk-summation.
After a median follow-up of 5.4 years, they found that asymptomatic AR patients are at low risk for mortality, with a 10-year survival similar to that of an age- and sex-matched general population. There was also an inverse association between age and LVESVi, but not LVESDi.
Additional results from Yang and colleagues included the following:
- LVESVi and Vol-LVEF were independently associated with death under surveillance, as were LVEF and LVESDi (all P<0.046).
- In patients with linear LVEF and Vol-LVEF <60%, the continuous risks of death increased, as it did for an LVESVi >40-45 mL/m2 and LVESDi >21-22 mm/m2.
- Patients with an LVESVi of more than 45 mL/m2 had an increased relative risk of death (HR: 1.93; 95% CI: 1.10-3.38; P=0.02), but those with an LVESDi greater than 20 mm/m2 did not (95% CI: 0.78-2.10; P=0.32).
- Finally, an LVESVi >45 mL/m2 carried a decreased survival trend compared with expected population survival.
Limitations of the study include that it was retrospectively done in a single tertiary referral center in a low-risk cohort, the inclusion of patients with atypical symptoms, and the inclusion of a small number of patients in whom LV volume could not be measured.
“Our results should not be interpreted as suggesting that conventional LV indexes (linear LVEF, LVESDi) are inferior to volume-derived parameters, but rather, that all 4 parameters offer opportunities to identify patients at risk of excess death in a low-risk asymptomatic AR population,” Yang and colleagues added.
In an accompanying editorial, Robert O. Bonow, MD, MS, editor of JAMA Cardiology, and of Northwestern University Feinberg School of Medicine in Chicago, and Patrick T. O’Gara, MD, of Brigham and Women’s Hospital, Boston, hailed these results as “an important step forward” in the care of patients with asymptomatic moderate/severe AR.
“Echocardiographic laboratories for several years have reported LV volumes, and the American Society of Echocardiography and European Society of Cardiovascular Imaging (ASE/ ESCVI) have jointly published criteria for severity of LV dilation based on LV end-systolic volume index (LVESVi). However, guideline recommendations for surgery remain based on linear measurements of LVESD and LVESDi using technology 30 to 40 years old, since there has been insufficient outcomes evidence based on LV volumes,” they wrote.
Like Yang and colleagues, however, Bonow and O’Gara were careful to add that LVESVi and Vol-LVEF should not replace LVESDi.
“While the current analysis provides helpful metrics for use of LVESVi in chronic aortic regurgitation, it is noteworthy that LVESVi did not clearly outperform LVESDi regarding mortality risk. It would thus not be wrong for clinicians to continue to use LVESDi in decision-making, but with the proviso that this and previous studies indicate that outcomes may be optimized using lower LVESDi thresholds than the current guidelines’ recommendation of 25 mm/m2,” they concluded.
-
To identify mortality risks in asymptomatic patients with hemodynamically significant aortic regurgitation, LVESVi and Vol-LVEF are as effective as LVESDi and linear LVEF.
-
In asymptomatic AR patients, an LVESVi threshold of 45 mL/m2 or greater was associated with an increased mortality risk.
E.C. Meszaros, Contributing Writer, BreakingMED™
Yang and Bonow reported no disclosures.
O’Gara has served on the executive committees of the APOLLO Transcatheter Mitral Valve Replacement Trial for Medtronic and the EARLY TAVR trial for Edwards Life Sciences outside the submitted work.
Cat ID: 914
Topic ID: 74,914,914,192,925