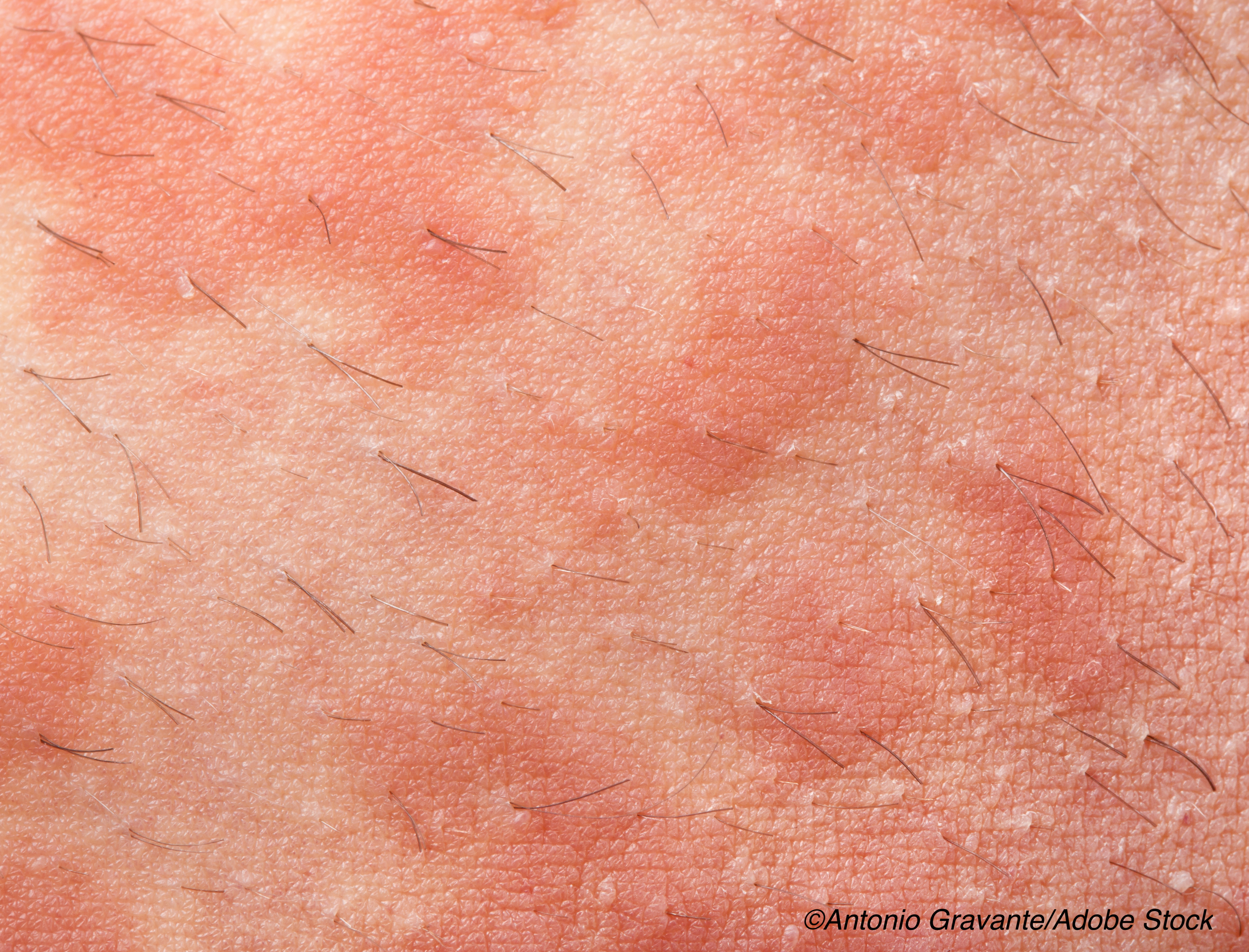
Bacteriotherapy using an autologous strain of coagulase-negative Staphylococcus in patients with atopic dermatitis (AD) effectively improved disease severity and safely decreased the colonization of Staphylococcus aureus on the skin, which is often problematic in these patients, according to researchers of a small, single-center study.
The researchers are hopeful that—after further clinical trials—this investigational therapeutic approach could change the course of AD, especially in affected children.
“Compared with individuals without AD, patients with AD lack coagulase-negative Staphylococcus (CoNS) that has the capacity to produce antimicrobials (AM) that inhibit SA (CoNS-AM+),” wrote Tissa Hata, MD, of the University of California, San Diego, and colleagues, in JAMA Dermatology. “In an effort to correct this defect, we previously demonstrated that a single application of autologous CoNS-AM+ reduced skin colonization by SA in AD skin. However, one application was not enough to show clinical improvement. Here, we hypothesize that extended treatment with autologous CoNS-AM+ for one week would be well tolerated and suppress SA survival in addition to promoting an improvement in each patient’s AD by correcting the defects in their skin microbiome.”
For this double-blind, vehicle-controlled, single-center, randomized, clinical trial, Hata and fellow researchers randomized 11 patients with moderate-to-severe AD to treatment with autologous CoNS-AM+ or vehicle. To obtain autologous CoNS-AM+, researchers swabbed unaffected skin on each AD patient, and isolated, cultured, and expanded these cells, which were then topically reapplied to the forearms at a concentration of 107 colony-forming units/g. Patients were treated for one week.
The primary endpoint of the study was the concentration of S. aureus one week after autologous CoNS-AM+ application as measured by culture and DNA testing; secondary endpoints included safety and clinical outcomes measures.
In patients treated with autologous CoNS-AM+, S. aureus colonization on lesional skin was significantly reduced (99.2%; mean of log10 ratio to baseline: −1.702; 95% CI: −2.882 to −0.523) compared with those treated with the vehicle (mean of log10 ratio to baseline: 0.671; 95% CI: −0.289 to 1.613; P=0.01), and this reduction lasted four days after treatment (CoNS-AM+: mean of log10 ratio to baseline: −1.752; 95% CI: −3.051 to −0.453; vehicle: mean of log10 ratio to baseline: −0.003; 95% CI: −1.083 to 1.076; P=0.03).
On day 11, local Eczema Area and Severity Index scores from patients treated with CoNS-AM+ improved significantly compared with those from patients treated with vehicle (mean percentage change: −48.45 vs −4.52; P=0.04).
“Early results from this study, as well as others, demonstrate promise for bacteriotherapy that utilizes protective skin commensal microbes in AD. Future investigations that target the microbiome in AD represent a therapeutic approach that may alter the pathogenesis of AD and explore its potential as an early intervention in pediatric AD,” Hata and colleagues concluded.
No serious adverse events occurred in either group, and only two mild adverse events—mild rash and stinging—occurred in each group.
Further, noted Hata et al, “Analysis of the absolute abundance of bacteria as measured by quantitative polymerase chain reaction for the 16S ribosomal RNA gene showed no difference on the lesional skin between the active- and vehicle-treated groups. These data suggest that the continued reapplication of live CoNS-AM+ was well tolerated and did not lead to accumulation of bacteria on the skin surface.”
Tamia A. Harris-Tryon, MD, of The University of Texas Southwestern Medical Center, Dallas, and Shai Bel, PhD, of Bar-Ilan University, Safed, Israel, commented on the importance of the skin microbiome in an accompanying editorial.
“Our skin hosts bacteria, viruses, fungi, and mites, with a unique repertoire of commensal microbes at oily, moist, dry, and acral sites. These organisms, collectively termed ’the microbiota,’ inhabit the skin surface and skin appendages, including hair follicles and sebaceous glands,” they wrote. “Clinical and preclinical studies have established an association between inflammatory skin diseases and imbalances in the microbiota. These associations underscore the key function that the microbiota play in disease pathogenesis and suggest that skin commensals may have therapeutic potential in the treatment of inflammatory skin diseases, such as atopic dermatitis (AD). In this issue of JAMA Dermatology, [Hata] and colleagues demonstrate that commensal species of Staphylococcus can shape the microbiota and improve disease severity in AD.”
Study limitations include its single-center design, small cohort, and inclusion of only patients with SA-positive AD.
-
Bacteriotherapy with an autologous strain of bacteria may safely improve colonization of Staphylococcus aureus in the microbiome of patients with AD and improve disease severity.
-
This investigational approach to the treatment of AD is promising and could prove particularly beneficial in children with AD.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
This study was funded by the National Institutes of Health.
Hata reported no disclosures.
Harris-Tryon and Bel reported no disclosures.
Cat ID: 449
Topic ID: 75,449,730,449,138,192,923,925