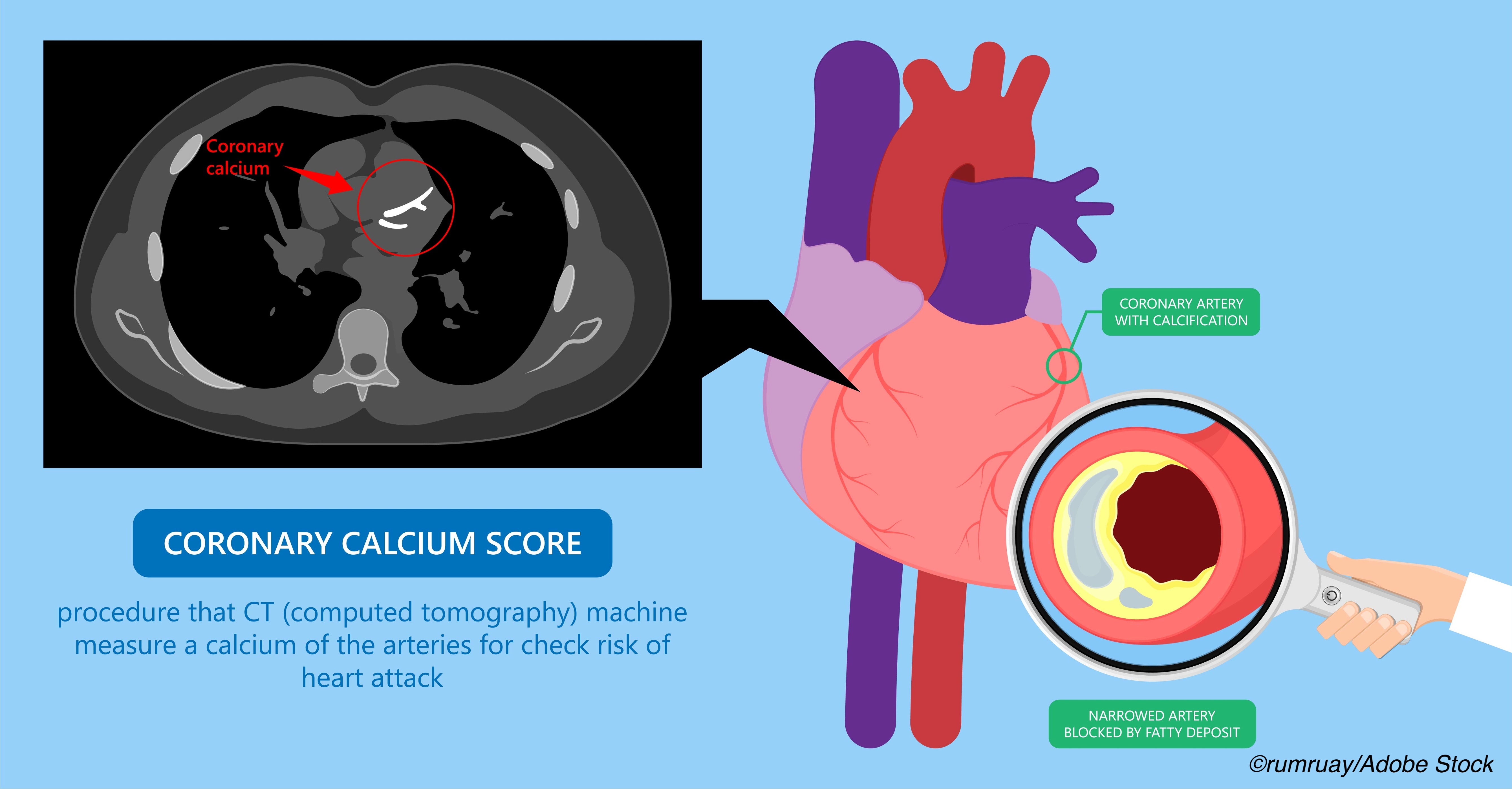
The risk of cardiovascular disease, particularly coronary artery disease, among breast cancer survivors is well-known, but a study from Dutch researchers suggests that CT scans used to plan breast cancer treatment regimens can also measure coronary artery calcium (CAC), and those CAC scores can be used to reduce the heart disease burden seen in breast cancer survivors.
The concept provides a real-world example of the interface between oncology and cardiology, which has given rise to cardio-onco subspecialists, and it offers the added advantage of simplicity: CAC scores can be “automatically extracted from planning CT scans using a deep learning algorithm.”
In this cohort study of 15,915 breast cancer patients who underwent CT planning scans prior to receiving radiotherapy and then followed for a median of 51.2 months, women with coronary artery calcium (CAC) scores of more than 400 had an increased risk of fatal and nonfatal cardiovascular disease (CVD) events, wrote Roxanne Gal, PhD, of the Division of Imaging and Cancer, Department of Radiotherapy University Medical Center Utrecht, Utrecht, the Netherlands, and colleagues in JAMA Oncology.
“A total of 11,179 (70.2%) patients had no CAC; 10% (n=1,584), 11.5% (n=1,825), 5.2% (n=830), and 3.1% (n=497) had CAC scores of 1 to 10, 11 to 100, 101 to 400, and greater than 400, respectively. Patients with higher CAC scores were on average older compared with patients without CAC,” Gal et al wrote.
After just over four years, 8.4% (n=1,341) of the cohort was hospitalized at least once for CVD disease and 113 patients died of CVD.
There was a direct linear relationship between CAC score and CVD events. “Five percent of the patients without CAC (n=579/11,179) had CVD during follow-up, against 28.2% of the patients with a CAC score higher than 400 (n=140/497). The incidence rate of CVD increased from 10.7 per 1000 person-years in patients without CAC to 77.8 per 1000 person years in patients with a CAC score higher than 400… Compared with patients without CAC, patients with a CAC score of 1 to 10, 11 to 100, 101 to 400, and greater than 400 had a 1.1, 1.8, 2.1, and 3.4 higher risk of fatal and nonfatal CVD, respectively.”
And when anthracycline treatment was combined with a CAC score higher than 400, the CVD risk was 5.8 times higher than that seen in anthracycline-treated patients with no evidence of CAC.
“The incidence rate of all-cause mortality increased from 10.9 deaths per 1000 person-years in patients without CAC to 52.8 deaths per 1000 person-years in patients with CAC levels higher than 400,” they wrote. “After adjustment, patients with a CAC score higher than 400 continued to have an increased mortality risk (HR=2.8; 95% CI, 2.3-3.4).”
The Dutch researchers point out that the association between CAC and CVD events suggests that pulling the CAC data during CT planning scans should be routine and women with evidence of CAC can then be referred for “complete CVD work up, lifestyle advice and/or initiation of cardioprotective-pharmacotherapy.”
Additionally, CAC could inform breast cancer treatment strategies, for example avoiding anthracycline therapy.
Earlier studies have suggested that CVD risk following radiotherapy for breast cancer is greater for left-sided radiotherapy than it is for right-sided, but in the study by Gal et al there was no difference between left- and right-sided radiation. One explanation for this is time: 51.2 months may not be long enough to “draw conclusions on a potential interaction between CAC and left-sided versus right-sided radiotherapy.”
Another limitation of the study was the decision to include only irradiated patients, so it was impossible to “compare the risk of CVD in patients who received radiotherapy with patients who did not.” Moreover, the study did not evaluate other cardiovascular risk factors such as smoking, obesity, and lack of physical exercise among the women included in the cohort.
Finally, they concluded that, “the presence and extent of CAC, as automatically quantified on routinely performed radiotherapy planning CT scans, is strongly associated with CVD and allows identification of patients at increased risk of CVD. Timely and accurate identification of high-risk patients might allow mitigation of cardiovascular risk, including management of CVD risk factors and switching to less cardiotoxic treatment regimens.”
-
A cohort study of women with breast cancer found a “strong association” between coronary artery calcium and cardiovascular disease, especially among women treated with anthracyclines and those who also received radiation.
-
Findings from this study suggest that scoring coronary artery calcium as part of CT planning scans might be useful in assessing CVD risk among breast cancer patients so that strategies to reduce CVD burden can be initiated.
Peggy Peck, Editor-in-Chief, BreakingMED™
The study was funded by the Dutch Cancer Society.
Gal had no conflict of interest disclosures.
Cat ID: 22
Topic ID: 78,22,730,308,914,22,935,192,925,480,482,96


