In a study of 373 women who had completed breast cancer treatment, five independent prognostic variables were identified that predicted lymphedema risk: mammographic breast density, body mass index (BMI), age, number of pathological lymph nodes, and the extent of axillary lymph node dissection (ALND) required, Jennifer Yin Yee Kwan, MD, Princess Margaret Cancer Center, Toronto, Ontario, and colleagues reported in JAMA Network Open.
The same variables also predicted the development of severe lymphedema, defined as a volume in excess of 500 mL, investigators added.
“To our knowledge, this study is the first to not only report the use of diagnostic mammographic breast density as a prognostic factor for lymphedema risk but also to provide volumetric estimates of lymphedema severity,” Kwan and colleagues observed.
“Understanding who is at greatest risk of lymphedema will facilitate monitoring, earlier disease diagnosis, and early initiation of therapies to decrease disease morbidity,” they added.
CRS Program
Participants had been referred to the Cancer Rehabilitation and Survivorship (CRS) Program at the Princess Margaret Cancer Centre in Toronto, Ontario between July 2018 and March 2020.
The median age of the cohort was 52.3 years (Interquartile Range [IQR], 45.9-60.1 years) and the median length of follow-up from breast cancer diagnosis was 1.1 years (IQR, 0.6-2.5 years).
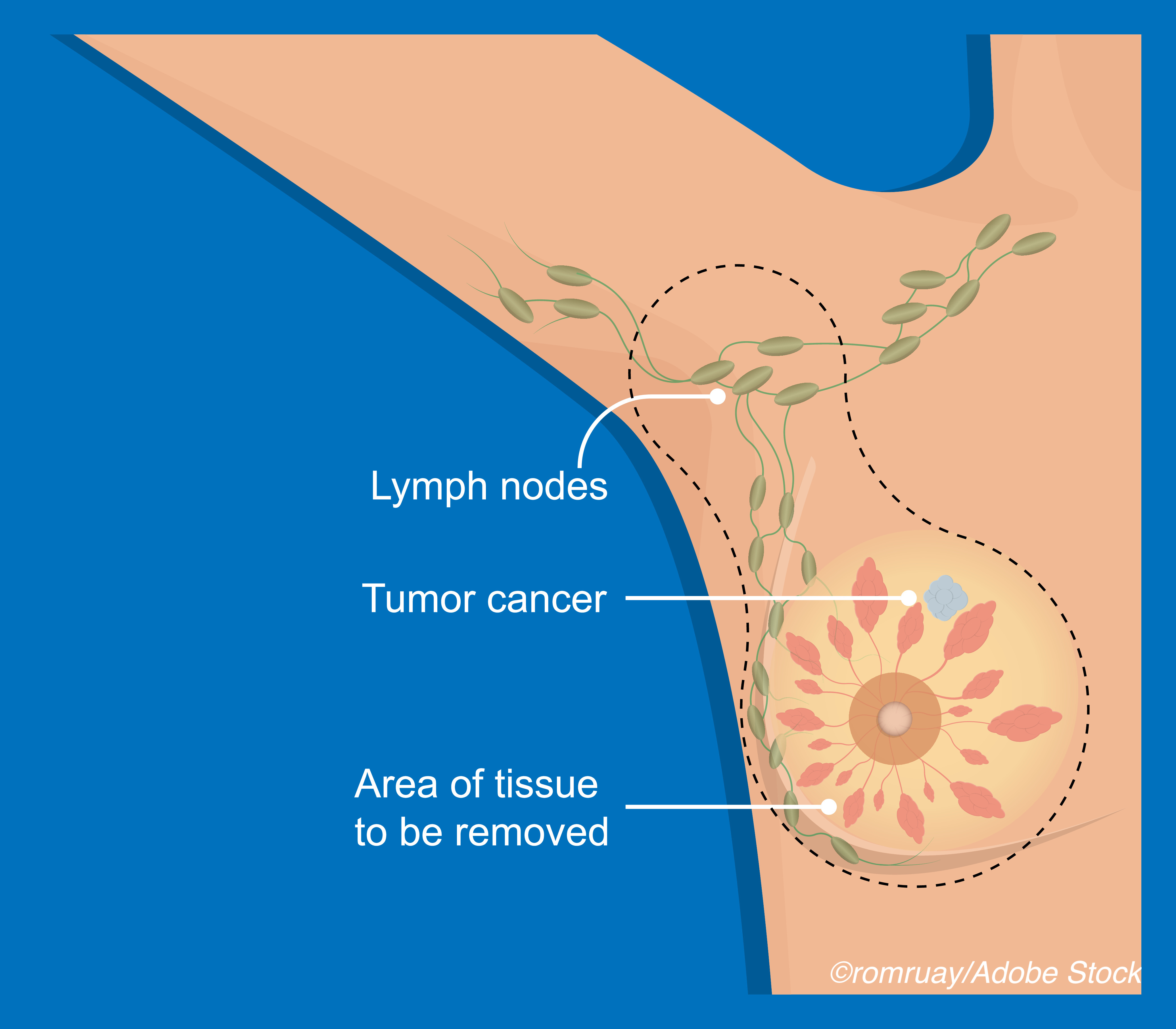
As the authors explained, in lymphedema, the lymphatic drainage system is damaged, which results in swelling and deformity of skin and adipose tissue. “To date, the main biological factor identified [for lymphedema] is high body mass index,” they wrote.
The main hypothesis of the study was that a more direct measurement of fat deposition, as reflected by findings from diagnostic mammography, would have a greater prognostic value in determining lymphedema risk than BMI.
The group was randomly split into a training cohort consisting of 247 patients and a validation cohort consisting of 126 patients. Comparing measured and predicted values of lymphedema volume, analyses revealed a statistically significant moderate correlation in both the training cohort (0.53; 95% CI, 0.43-0.62; P<0.001) and the validation cohort (0.42; 95% CI, 0.26-0.56; P<0.001), the investigators reported.
The area under the curve (AUC) values for predicting at least mild lymphedema were 0.81 (95% CI, 0.74-0.87) in the training cohort and 0.72 (95% CI, 0.60-0.83) in the validation cohort. “For severe lymphedema, the AUC values were 0.86 (95% CI, 0.78-0.93) in the training cohort and 0.83 (95% CI, 0.74-0.93) in the validation cohort,” they wrote and added that rates of lymphedema-free survival varied between those with predicted higher volumes of lymphedema compared to those with predicted lower volumes, investigators continued.
For patients with greater than a 200 mL predicted volume, the 2-year rate of lymphedema-free survival in the training cohort was only 58% (95% CI, 46%-74%) compared with 91% (95% CI, 85%-97%: P<0.001) for patients with predicted volumes of 200 mL or less.
The Hazard Ratio (HR) of actually developing high volume lymphedema in patients in whom high-volume lymphedema was predicted was 7.47 (95% CI, 3.92-14.2; P <0.001) in the training cohort.
“Similarly, in the validation cohort, the 2-year rate of lymphedema-free survival was 68% (95% CI, 53%-88%) in those with higher predicted volume versus 83% (95% CI, 74%-93%; P<0.41) in those with lower volume prediction,” at a HR of 2.39 (95% CI, 1.01-5.68: P=0.048), the researchers noted.
Risk Stratify Patients
Overall, the authors suggested that the use of their clinical prediction model will allow clinicians to risk stratify patients into clinically relevant groups, the first group being patients who are unlikely to develop any lymphedema following breast cancer treatment for whom routine follow-up care is likely all that will be needed.
For those who are predicted to develop either limited or mild lymphedema, patients can be encouraged to exercise more and lose weight as well as undergo more frequent monitoring in order to initiate the use of conservative therapies early on such as compression therapies. Moreover, patients who are predicted to develop severe lymphedema may be candidates for additional surgical interventions which are typically more successful before patients develop fibrosis, a feature of chronic lymphedema.
“[S]tudy results revealed that fatty breasts co-occurred with worse lymphedema, and on multivariate analysis, breast density added an independent prognostic value beyond BMI,” the authors stated. “[Since m]ammography is currently the standard of care for breast cancer screening and diagnosis… these data are readily available for inclusion in risk modeling.”
Commenting on the prediction model, Maggie Lee DiNome, MD, David Geffen School of Medicine, University of California, Los Angeles, pointed out that higher fat content in the breast, as reflected by The Breast Imaging Reporting and Data System (BI-RADS) scoring system, is actually associated with a lower risk of breast cancer.
However, according to the current study’s findings, the same fatty composition in the breast was associated with an increased risk of lymphedema, an association that might be explained by impaired adipose homeostasis in the breast following surgery accompanied by compromised lymphatic vasculature, as the authors also suggested.
“The de-escalation of ALND has been driven in large part by the recognition that this procedure results in the development of lymphedema in nearly 25% of patients,” DiNome noted. Nevertheless, ALND remains the standard of care for patients with clinically node-positive disease or for those whose cancer was not downstaged by neoadjuvant chemotherapy. She added, “The ability to better predict the risk of lymphedema in these patients is essential not only for appropriate counseling but also for earlier identification and intervention to mitigate the risk of developing this potentially disabling complication.”
-
Readily available clinical factors, including mammographic breast density information, predicted the risk of developing lymphedema after breast cancer treatment, as well as the severity of that risk.
-
This new clinical prediction model will allow clinicians to identify patients at risk for lymphedema after breast cancer treatment and tailor their interventions earlier to improve patient outcomes.
Pam Harrison, Contributing Writer, BreakingMED™
The authors reported no financial conflicts of interest.
DiNome had no conflicts of interest to disclose.
Cat ID: 22
Topic ID: 78,22,22,691,192,925


