Among patients hospitalized with severe Covid-19 not requiring mechanical ventilation, treatment with the anti-interleukin 1β monoclonal antibody canakinumab was not associated with increased survival, compared to placebo, in the phase III CAN-COVID clinical trial.
In addition, no significant difference in Covid-19-related mortality was observed between the canakinumab- and placebo-treated patients in the multicenter, randomized study, which was published online July 20 in JAMA.
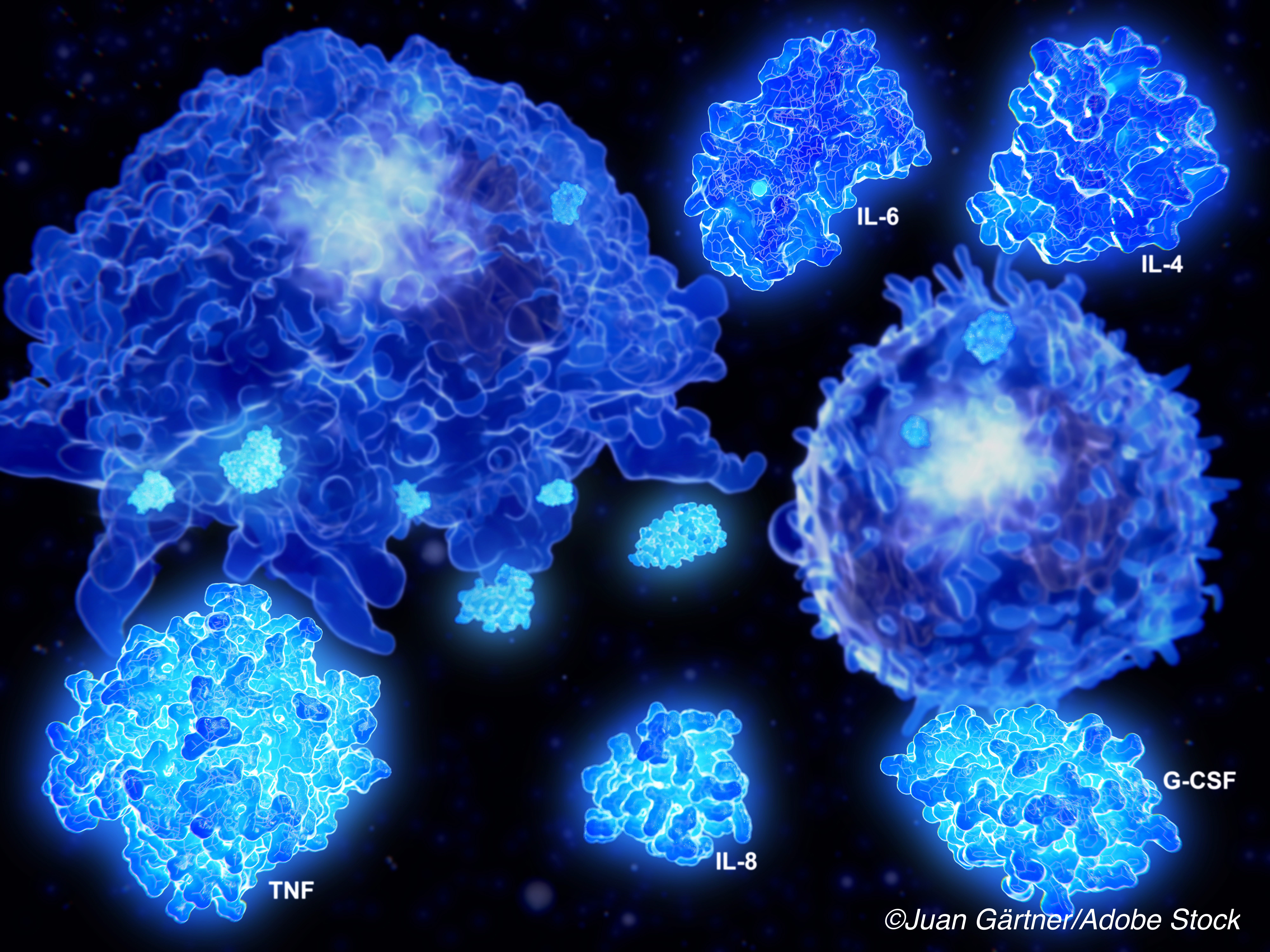
In conditions such as macrophage activation syndrome, IL-1 inhibition has been shown to inhibit inflammatory responses in patients with systemic hyperinflammation and cytokine storm, which can occur in severe Covid-19. The mechanism is thought to be inhibition of downstream mediators, including IL-6.
CAN-COVID researcher Roberto Caricchio, MD, of Philadelphia’s Lewis Katz School of Medicine at Temple University, and colleagues, noted that IL-1β is an upstream proinflammatory cytokine that is involved in the pathogenesis of many auto-inflammatory conditions, including IL-6.
They added that, “immunoprofile studies have shown that IL-1β is one of the inflammatory cytokines that defines the ’core Covid-19 signature.’”
To test their hypothesis that canakinumab could improve outcomes among patients hospitalized with severe Covid-19, Caricchio and colleagues conducted their phase III, double-blind randomized trial involving 454 patients being treated at 39 hospitals in Europe and the United States between April 30 and Aug. 17, 2020.
All recruited patients were experiencing hypoxia at enrollment, without the need for invasive mechanical ventilation (IMV), as well as systemic hyperinflammation. Most of the patients were receiving oxygen therapy by mask or nasal prongs at baseline.
The patients were randomly assigned 1:1 to receive a single intravenous infusion of canakinumab (450 mg for body weight of 40 to <60 kg, 600 mg for 60-80 kg, and 750 for >80 kg; n = 227) or placebo (n = 227). The study’s primary outcome was survival without IMV from day 3 to day 29. Secondary outcomes included Covid-19-related mortality and systemic hyperinflammation measures.
The mean age of the patients recruited for the study was 59 years, and 41.2% were female. A total of 417 (91.9%) completed day 29 of the trial.
Among the main findings:
- A total of 88.8% of patients treated with canakinumab and 85.7% of patients treated with placebo were alive without the need for IMV between study days 3 and 29, for a statistically insignificant rate difference of 3.1% (95% CI, −3.1% to 9.3%) and an odds ratio of 1.39 (95% CI, 0.76 to 2.54; P=0.29).
- Eleven (4.9%) of the canakinumab-treated patients completing the study, compared to 16 (7.2%) of placebo-treated patients died of Covid-19, for a rate difference of −2.3% (95% CI, −6.7% to 2.2%) and an odds ratio of 0.67 (95% CI, 0.30 to 1.50).
- By day 29, 35.2% of patients in the canakinumab group and 30.4% of patients in the placebo group had no clinical or virologic evidence of infection. No significant differences in the rate of hospital discharge over time were observed between the two groups.
- Serious adverse events occurred in 36 (16%) of evaluated canakinumab-treated patients and 20.6% of patients in the placebo group, with one patient (o.4%) in the active-treatment arm and no patients in the placebo arm requiring discontinuation of the study drug.
A significant study limitation cited by the researchers was the fact that the study was designed and begun early in the Covid-19 pandemic, as the treatment standard-of-care was evolving. They noted that prior to recruitment, more patients randomized to receive canakinumab were treated with dexamethasone and these patients were also more likely to receive study-prohibited medications (tocilizumab and anakinra) prior to recruitment.
And, as the study progressed, the mortality and morbidity outcomes became more favorable “likely due to a better understanding of the disease and its management,” the researchers wrote.
“These challenges underscore the difficulty in conducting randomized clinical trials in the changing treatment approach during the Covid-19 pandemic,” they concluded. “These shortcomings may be best addressed in the future by event-driven trial designs.”
-
Among patients hospitalized with severe Covid-19 not requiring mechanical ventilation, treatment with the anti-interleukin 1β monoclonal antibody canakinumab was not associated with increased survival, compared to placebo.
-
No significant difference in Covid-19-related mortality was observed between the canakinumab- and placebo-treated patients in the multicenter, randomized CAN-COVID study.
Salynn Boyles, Contributing Writer, BreakingMED™
This study was sponsored by Novartis Pharma AG. Caricchio received grants from Janssen and personal fees from Janssen, Glaxo-SmithKline, Bristol Myers Squibb, Eli Lilly and Siemens outside the submitted work. Principal investigator Stephanie Noviello reported being a former employee and stokholder of Bristol Myers Squibb and a stokholder of Johnson & Johnson. Dr. Noviello also reported having a patent pending through Novartis.
Cat ID: 190
Topic ID: 79,190,730,933,190,926,192,927,151,928,925,934