Non-White patients with atrial fibrillation (AFib) had clinical outcomes significantly improved after treatment with catheter ablation compared with drug therapy alone, according to a recent subgroup analysis of data from the Catheter Ablation Versus Antiarrhythmic Drug Therapy for Atrial Fibrillation (CABANA) trial.
Looking only at participants enrolled in North America, the researchers found catheter ablation resulted in significant reductions in the primary composite endpoint of death, disabling stroke, severe bleeding, cardiac arrest, as well as in all-cause mortality in non-White patients. Researchers concluded that these clinical benefits were most likely due to worse outcomes with drug therapy. Their results are published in the Journal of the American College of Cardiology.
“The 2014 American College of Cardiology, American Heart Association, and Heart Rhythm Society updated guidelines support a more prominent role for catheter ablation in the treatment of atrial fibrillation (AFib), including its use as first-line therapy for recurrent symptomatic paroxysmal or persistent AFib. Historically, Blacks and other racial and ethnic minorities have been underrepresented in clinical trials focused on the management and treatment of AFib. Observational data indicate lower use of rhythm control strategies, including catheter ablation, in the management of AFib among racial and ethnic minorities, and there are no randomized trial data describing the safety and efficacy of catheter ablation therapy to treat AFib in these patients,” wrote researchers led by Kevin L. Thomas, MD, of the Duke Clinical Research Institute, Duke University, Durham, North Carolina.
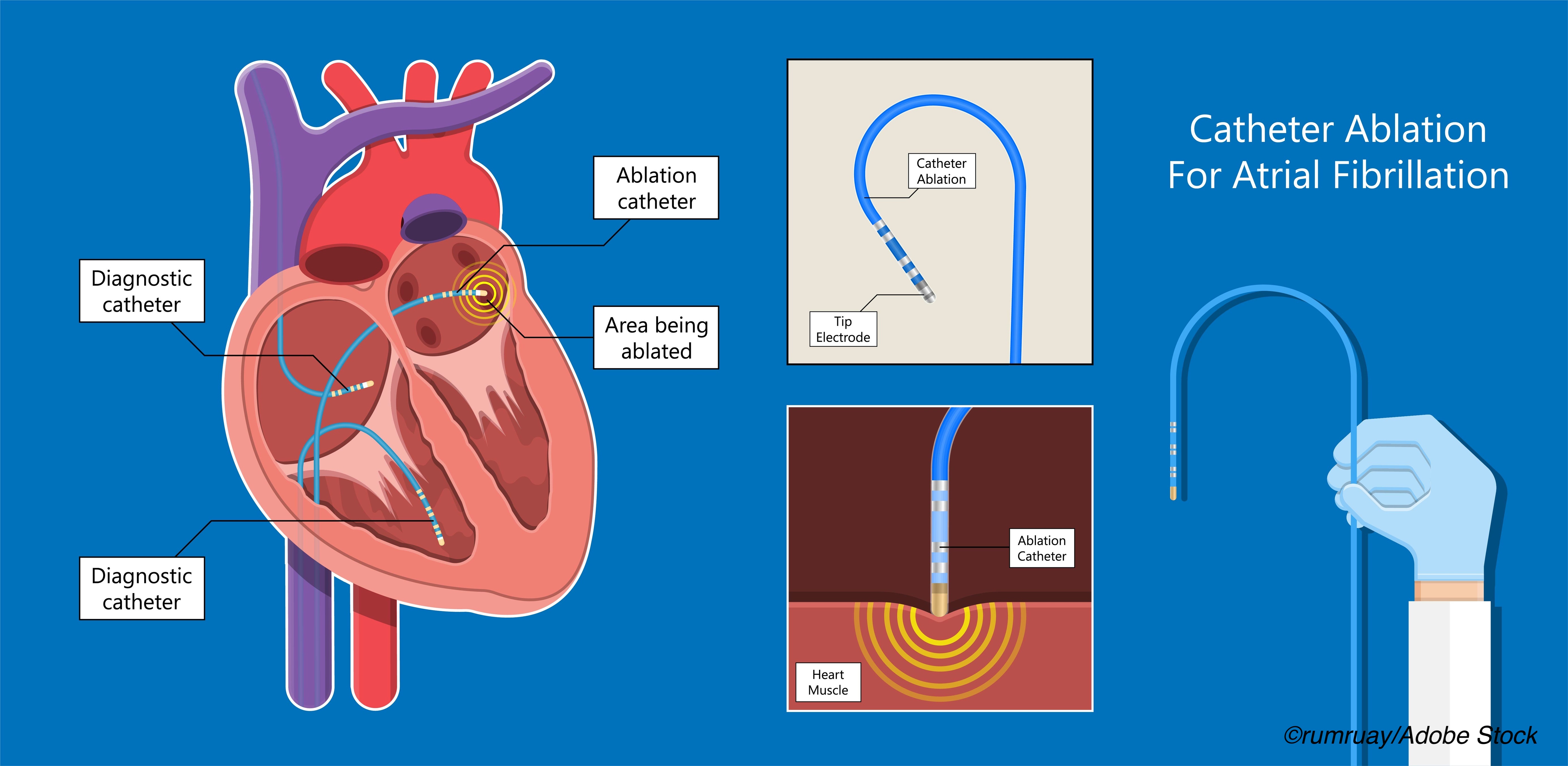
In the main CABANA trial, 2,204 patients with symptomatic atrial fibrillation were randomized to catheter ablation or pharmacologic treatment with rate and/or rhythm control agents.
“The CABANA (Catheter Ablation Versus Antiarrhythmic Drug Therapy for Atrial Fibrillation) trial, the largest trial to date of catheter ablation versus drug therapy in AFib, found that the strategy of catheter ablation did not significantly improve the composite primary clinical outcome (death, disabling stroke, serious bleeding, or cardiac arrest) compared with drug therapy when analyzed by intention to treat. Secondary endpoints of death or cardiovascular hospitalization, as well as AFib recurrence, were significantly reduced by ablation, and quality of life was improved out to 60 months. The objective of the present analysis was to assess if the response to treatment assignment in CABANA varied according to minority race or ethnicity among patients enrolled in North America (NA),” they explained.
In their analysis, Thomas et al included only North American patients from the CABANA trial, whom they grouped into racial/ethnic minority or nonminority subgroups and randomized to treatment with catheter ablation or drug therapy alone. In all, 62 racial/ethnic minority patients and 587 non-minority patients underwent ablation, while 65 and 566, respectively, were randomized to drug therapy.
The primary endpoint was a composite of death, disabling stroke, serious bleeding, or cardiac arrest, and patients were followed for a median of 54.9 months.
Of the 1,280 North American patients, 127 belonged to racial and ethnic minorities and 1,153 were nonminority patients. Those who belonged to racial and ethnic minorities were younger than nonminority patients (median age: 65.6 vs 68.5 years, respectively), and evidenced more symptomatic heart failure (37.0% vs 22.0%), hypertension (92.1% vs 76.8%) and ejection fractions less than 40% (20.8% vs 7.1%).
Patients who belonged to racial or ethnic minorities and were treated with ablation experienced a 68% relative reduction in the primary endpoint (adjusted HR [aHR]: 0.32; 95% CI: 0.13-0.78) as well as a 72% relative reduction in all-cause mortality (aHR: 0.28; 95% CI: 0.10-0.79).
In the ablation arm, the incidence of primary events between racial and ethnic minorities and nonminority patients was similar (4-year Kaplan-Meier event rates: 12.3% vs 9.9%, respectively). But racial and ethnic minority patients randomized to drug therapy had a significantly higher event rate compared with nonminority patients (27.4% vs 9.4%).
Death or cardiovascular hospitalization occurred in 59.7% of patients in the catheter ablation arm, compared with 69.2% of those in the drug therapy arm, and death from cardiovascular causes was seen in 3.2% vs 10.8%, respectively.
“Racial and ethnic minorities in the drug arm had an early acceleration of mortality during the first 12 months following randomization, which accounted for most of the excess events producing the discrepancy with nonminority drug arm participants,” wrote Thomas and colleagues.
In an accompanying editorial, Andrea M. Russo, of Cooper University Hospital, Camden, New Jersey, stressed that historically, racial and ethnic minorities are consistently less likely to be treated with rhythm control strategies, particularly catheter ablation. She added that the results obtained by Thomas and colleagues were much different than those of the original CABANA trial.
“Although there was no significant difference in the primary composite endpoint of death, disabling stroke, serious bleeding, or cardiac arrest for ablation and drug therapy groups in the main CABANA trial, racial and ethnic minorities treated with ablation demonstrated a 68% relative reduction in the primary endpoint (adjusted hazard ratio [aHR]: 0.32; 95% CI: 0.13-0.78),” she wrote.
Yet, like Thomas et al, Russo also noted that the advantage of ablation was cause by the worse outcomes in patients treated with drug therapy alone. Yet, she concluded:
She concluded: “Thomas et al should be commended on reporting outcomes in a diverse North American population of patients undergoing ablation versus drug therapy in a large randomized clinical trial. These findings further highlight the importance of enrolling a racially and ethnically diverse group of subjects in clinical trials, because outcomes may not necessarily be generalizable to all subgroup. These findings further highlight the importance of enrolling a racially and ethnically diverse group of subjects in clinical trials, because outcomes may not necessarily be generalizable to all subgroups…This paper should be a “call to action” to ensure that all treatment options, including catheter ablation, are widely accessible to provide the highest quality of care for all patients with AFib.”
Study limitations include the underrepresentation of each racial and ethnic minority, as well as the combination of them without distinctions, and the lack of data on cultural differences and care delivery. Thomas and colleagues also noted “…the possibility exists that the unexpected higher mortality rate in the racial and ethnic minority drug arm patients may represent, at least in part, an adverse interaction between one or more rhythm control drugs, hypertensive myocardial disease, and symptomatic HF. Our sample size is too small to allow the interaction of these factors to be evaluated.”
-
Catheter ablation is safe and possibly more effective than antiarrhythmic drug therapy alone for patients from racial and ethnic minority groups with atrial fibrillation.
-
Patients from racial and ethnic minorities who were treated with catheter ablation demonstrated a 68% relative reduction in the primary endpoint, which was a composite of death, disabling stroke, severe bleeding, and cardiac arrest.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
This work was supported by the National Institutes of Health, St. Jude Medical Foundation and Corporation, Biosense Webster, Medtronic, and Boston Scientific Corporation.
Thomas has received grants from the National Heart, Lung, and Blood Institute (National Institutes of Health), Patient-Centered Outcomes Research Institute, and American Heart Association; and has received consulting fees from Sanofi, Boehringer Ingelheim, Janssen, Bristol Myers Squibb, and Medtronic during the conduct of the study.
Russo has received research funding from Boston Scientific, Kestra, and Medilynx; is on the research steering committees for Boston Scientific and Medtronic; and has received consulting fees from Biosense Webster, Boston Scientific, and Medtronic.
Cat ID: 2
Topic ID: 74,2,730,2,913,192,925



Create Post
Twitter/X Preview
Logout