1. Compared to population- and sibling-matched cohorts, women previously diagnosed with cervical intraepithelial neoplasia grade 3 were more likely to have adverse pregnancy outcomes.
2. These adverse outcomes include higher risks of preterm birth, infection, and neonatal death.
Evidence Rating Level: 2 (Good)
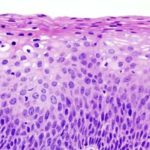
Study Rundown: Extensive screening and prompt treatment have been standard-of-care for high-grade cervical intraepithelial neoplasia (CIN). While this strategy was well adopted, concerns of overtreatment arise since many CINs were treated without additional biopsies. This is especially pertinent in women of reproductive age since treatment involves a surgical intervention to the cervix, which could potentially affect future pregnancies. The current cohort study examined the pregnancy outcomes of women in Sweden who had previously been diagnosed and treated for CIN grade 3 (CIN 3) and compared these to their population- and sibling-matched counterparts without a prior CIN 3 diagnosis. It was observed that women with prior CIN 3 had a higher risk of adverse pregnancy outcomes, such as preterm births, chorioamnionitis, infant sepsis, and neonatal deaths, compared to the general population and their siblings. This risk difference, however, narrowed as the time of delivery passed. Since CIN 3 has always been treated in Sweden, the study could not determine how CIN treatment impacted these outcomes. Nonetheless, its results showed an association between CIN 3 and adverse pregnancy outcomes, which was independent of family factors.
Click here to read the study in Annals of Internal Medicine
Relevant Reading: Adverse Pregnancy Outcomes After Treatment for Cervical Intraepithelial Neoplasia
In-Depth [retrospective cohort]: The article reported results from a population- and sibling-matched cohort study examining the association between CIN 3 diagnosis and pregnancy outcomes in Sweden. For the population comparison, the study examined 78,450 singletons born to women previously diagnosed and treated for CIN 3; 748,500 matched singletons born to women without previous CIN 3 history. For the sibling comparison, 23,199 singletons born to women with CIN 3 history were matched to 28,135 singletons born to their sisters without CIN 3. Match criteria included age at delivery, parity, years of education, preeclampsia status, marital status, smoking in pregnancy, and pre-pregnancy body mass index (BMI). The pregnancy outcomes of interest include preterm birth (categorized as extremely, very, or moderately), chorioamnionitis, infant sepsis, small size for gestational age, and fetal or neonatal deaths. Overall, compared to the general population women with CIN 3 history were more likely to have a preterm birth (<37 weeks) (odds ratio [OR], 2.09; 95% confidence interval [CI], 2.03 to 2.15); especially an extremely preterm birth (22-28 weeks) (OR, 3.00; 95% CI, 2.69 to 3.34). Chorioamnionitis (OR, 3.23; 95% CI, 2.89 to 3.62), infant sepsis (OR, 1.72; 95% CI, 1.60 to 1.86), neonatal death (OR, 1.83; 95% CI, 1.61 to 2.09) were also more likely in women with CIN 3 history. Comparison with matched siblings yielded similar associations. Furthermore, these associations were stronger in women with lower educational backgrounds, higher parity, and lower pre-pregnancy BMI. These elevated risks attenuated as the time of delivery passed, especially with the risk of neonatal death, suggesting that the modern more conservative CIN 3 treatment could decrease adverse pregnancy outcomes. The study noted that all CINs 3 were treated in Sweden and therefore, it could not determine the independent impact CIN 3 diagnoses and treatments had on pregnancy outcomes. These results suggested that women with a history of CIN 3 should be considered “high risk” in their pregnancies and receive appropriate management.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.