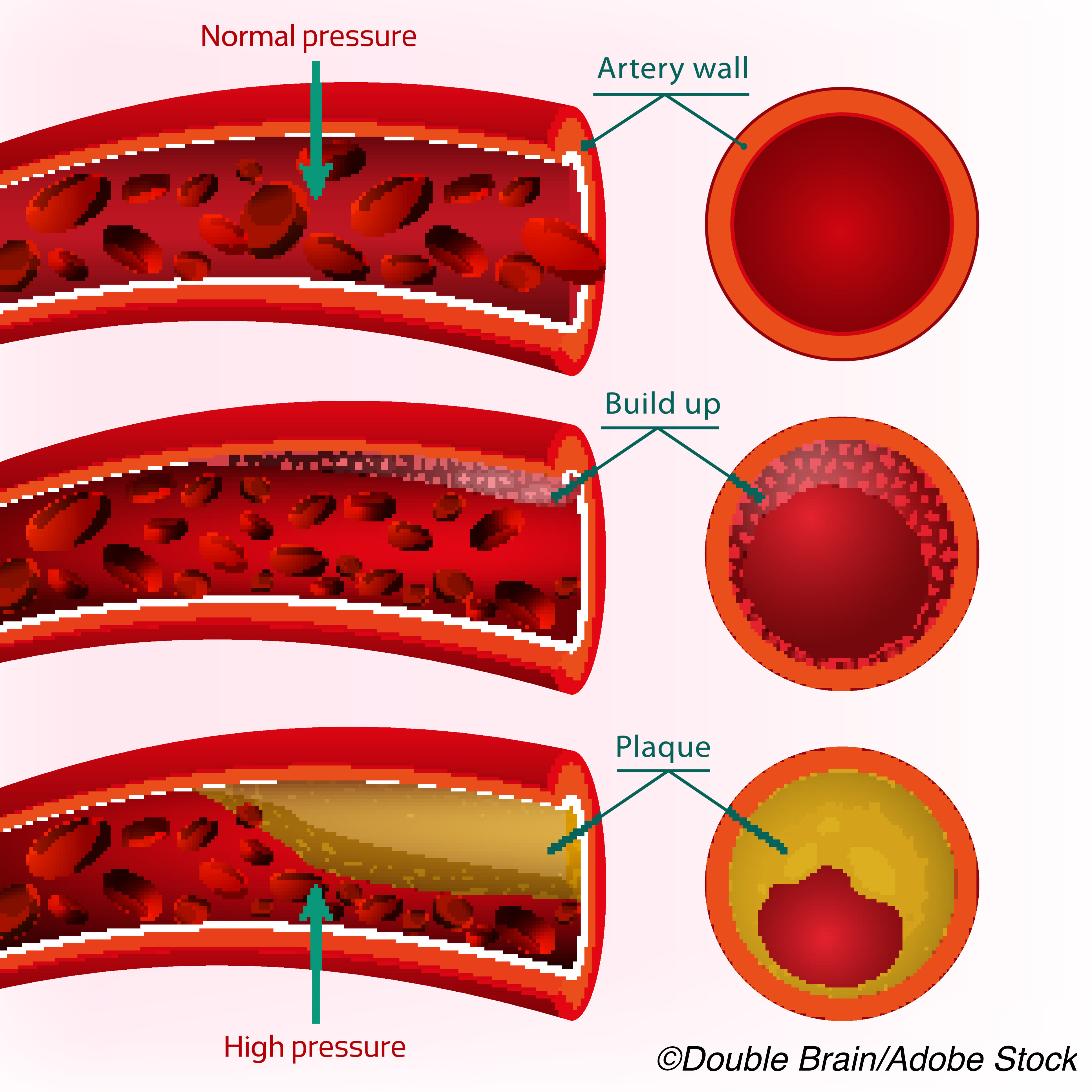
“Plaque burden, not stenosis per se, is the main predictor of risk for CVD events and death,” wrote Martin Bodtker Mortensen, MD, PhD, of Aarhus University in Denmark, and coauthors in the Journal of the American College of Cardiology.
Myocardial infarction, stroke, and all-cause death in 23,759 symptomatic patients from the Western Denmark Heart Registry were predicted similarly by CAC score (6.2 events per 1,000 person-years when CAC=0, and 42.3 events per 1,000 person-years for CAC >1,000) and the number of vessels with obstructive disease (6.1 events per 1,000 person-years for no CAD, and 34.7 per 1,000 person-years for three-vessel disease), they reported.
For each level of stratified CAC score, risk increased in stepwise fashion and was similar for those with and without vessel stenoses of 50% or more.
The study “adds significantly to the growing published data suggesting that it is the overall coronary plaque burden, not just stenosis, that provides a more complete assessment of patient risk,” noted Todd Villines, MD, and Patricia Rodriguez Lozano, MD, of the University of Virginia in Charlottesville, in an accompanying editorial.
“It is time that the traditional definitions of primary and secondary prevention evolve to incorporate CAC and CTA measures of patient risk based on coronary artery plaque burden,” they wrote. “Atherosclerotic cardiovascular disease risk parallels the amount of atherosclerosis, regardless of stenosis or prior revascularization procedures.”
A 2016 review summarized emerging concerns about the limitations of stenosis alone as a risk barometer for all patients who would go on to have cardiac events: “Patients undergoing coronary angiography for suspected coronary heart disease who are found to have coronary atherosclerotic disease with <50% diameter stenosis may carry a risk of adverse cardiac events similar to that in patients with single-vessel obstructive disease.”
Coronary CTA uses contrast medium to identify lumen stenosis; the same imaging session can be used to obtain additional data and calculate a variety of scores, including non-contrast image based CAC score, a marker of plaque burden. A prospective randomized trial found 16% of patients with CAC=0 had evidence of noncalcified coronary atherosclerosis, and accounted for 16% of events.
The question of whether measures of plaque burden are superior to lumen stenosis for event prediction in symptomatic patients “has never been more important given the recent ISCHEMIA trial that demonstrated medical therapy should be the preferred approach in most patients with stable coronary heart disease presentations,” the editorialists pointed out.
In their study, Mortensen and colleagues included adult patients who had CTA between January 2008 and December 2018 due to CAD-suggestive symptoms. The primary endpoint was combined MI, stroke, or all-cause death occurring >90 days after the CTA until the end of follow-up. Events occurring within 90 days were excluded.
Mean age of the cohort overall was 57 and about 45% were male. No or nonobstructive disease was seen in 18,716 and obstructive disease in 5,043. Most participants had no detectable CAC (53%). Any stenosis of 50% or more was seen in 21%, and <2% had 3-vessel obstructive disease.
Of those with a CAC score of 0, about 13% had some coronary atherosclerosis, and 6% had 50% or more stenosis. Both the prevalence of obstructive CAD and the number of vessels with obstructive disease increased with calcified atherosclerotic burden.
Over median follow-up of 4.3 years, 1,054 patients had a first major CVD event: myocardial infarction (n=219), stroke (n=299) and death (n=536).
“We observed a stepwise increase in risk with both increasing calcified atherosclerotic burden and number of vessels with obstructive CAD,” the researchers wrote. “However, when stratified by calcified atherosclerotic burden, the risk of major CVD events was comparable in patients with obstructive and nonobstructive CAD.”
“Going forward, guidelines and the way clinicians discuss and address risk should incorporate the important prognostic data obtained from whole-heart atherosclerotic imaging provided by contrast and noncontrast cardiac CT,” the editorialists suggested. “It should come as no surprise that for the prediction of atherosclerotic cardiovascular events, atherosclerotic plaque burden, regardless of stenosis, probably matters most.”
A limitation of the study includes a strong correlation between CAC severity and significant stenosis. “Although stenosis did not add to CAC for prognostic purposes, the converse is also likely true and was not reported; that for each level of stenosis severity, CAC likely did not add prognostic value either,” the editorialists noted.
“The authors did not assess numerous other well-validated measures of coronary plaque burden that are routinely obtained from coronary CTA that typically improve the prognostic accuracy of coronary CTA beyond stenosis alone,” they added.
-
Scores of coronary artery calcium (CAC), a measure of plaque burden defined on non-contrast CT images, predicted major cardiovascular events almost as well as stenosis defined by CT angiography (CTA) in patients with coronary artery disease (CAD), a retrospective observational study found. However, of those with a CAC score of 0, about 13% had some coronary atherosclerosis, and 6% had 50% or more stenosis.
-
A limitation is the strong correlation between CAC severity and significant stenosis. “Although stenosis did not add to CAC for prognostic purposes, the converse is also likely true and was not reported; that for each level of stenosis severity, CAC likely did not add prognostic value either,” the editorialists noted.
Paul Smyth, MD, Contributing Writer, BreakingMED™
This study was funded by Aarhus University Hospital.
Mortenson had no disclsoures.
Villines is a past-president and member of the board of directors of the Society of Cardiovascular Computed Tomography.
Cat ID: 308
Topic ID: 74,308,308,914,192,925


