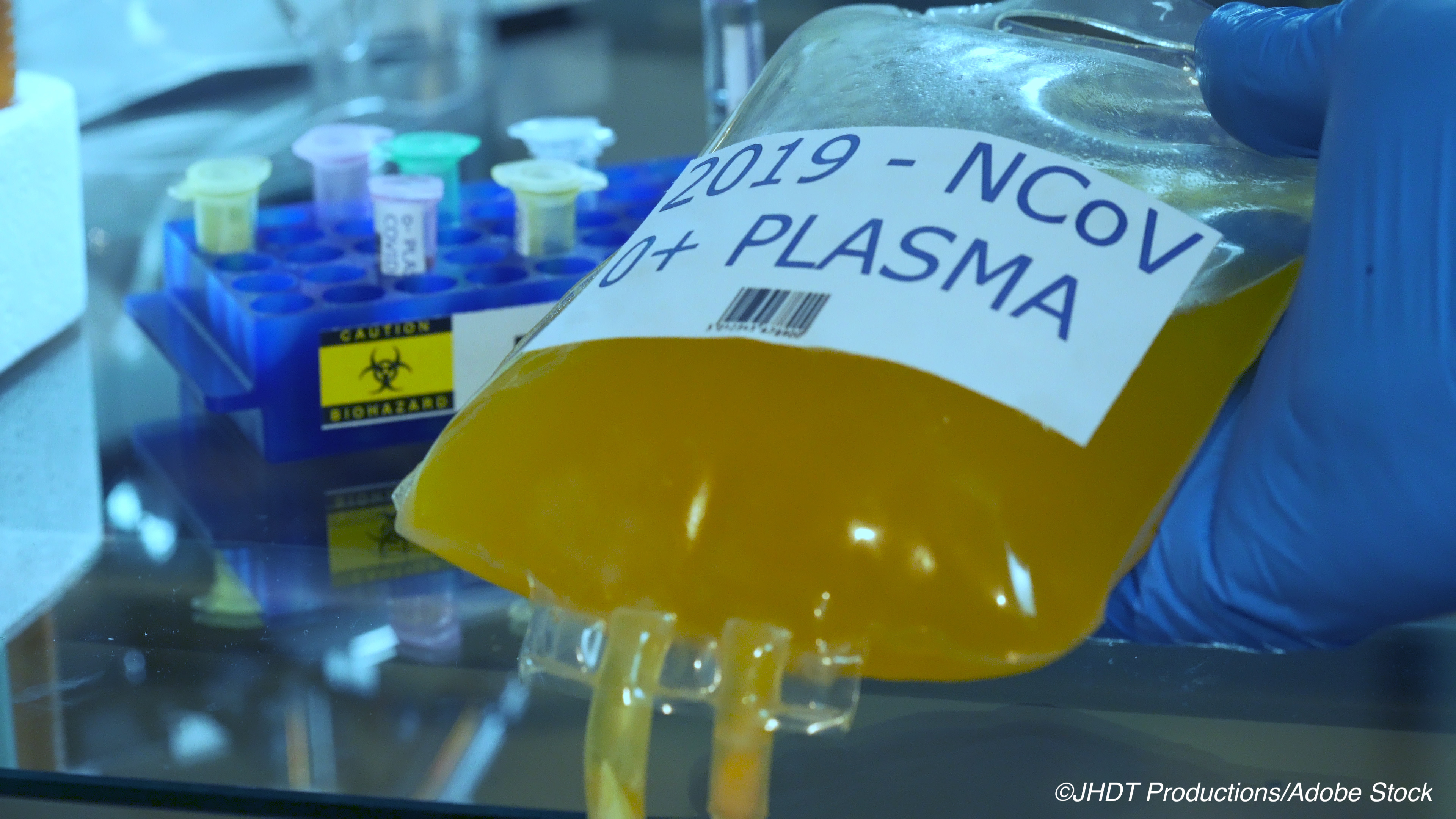
Convalescent plasma did not show benefit over placebo in the treatment of patients with severe Covid-19, according to the results of a double-blind, placebo-controlled, randomized trial published in the New England Journal of Medicine.
Convalescent plasma has gained attention as a potential treatment for Covid-19 based on observational studies, which have shown its safety — and, some of the studies, such as this one from the Mayo Clinic, showed efficacy for patients who received convalescent plasma within 3 days of diagnosis. However, the efficacy of convalescent plasma has not been evaluated in robustly powered randomized trials.
“In an attempt to more clearly determine the effect of convalescent plasma in Covid-19, we planned and conducted the PlasmAr trial to evaluate the safety and efficacy of convalescent plasma in the treatment of SARS-CoV-2 pneumonia,” Ventura A. Simonovich, MD, Clinical Pharmacology Section, Department of Internal Medicine, and the Department of Research Hospital Italiano de Buenos Aires, Argentina, and colleagues wrote. “The main hypothesis of this trial was that in patients with severe SARS-CoV-2 pneumonia, treatment with convalescent plasma would be associated with improved clinical outcomes at 30 days.”
Simonovich and colleagues randomized patients to either convalescent plasma (n=228) or placebo (n=105). The patients’ median time to enrollment in the trial was 8 days from symptom onset, “and hypoxemia was the most frequent severity criterion for enrollment.” The study authors also noted that “the infused convalescent plasma had a median titer of 1:3200 of total SARS-CoV-2 antibodies (interquartile range, 1:800 to 1:3200).”
Enrollment criteria included confirmed positivity for SARS-CoV-2 via reverse-transcriptase–polymerase-chain-reaction (RT-PCR) testing, radiologically confirmed pneumonia, no previous directives rejecting life support, and “at least one of the following severity criteria: oxygen saturation (SaO2) below 93% while they were at rest and breathing ambient air, a ratio of the partial pressure of oxygen (PaO2) to the fraction of inspired oxygen (FiO2) below 300 mm Hg (PaO2:FiO2), or a Sequential Organ Failure Assessment (SOFA) or modified SOFA (mSOFA) score of two or more points above baseline status (scores range from 0 to 24, with higher scores indicating more severe disease),” the study authors wrote.
During the trial, patients in either arm could receive antiviral agents, glucocorticoids, or both. Clinical status after intervention was the primary outcome. The median age of the patients in the trial was 62, most were male, and nearly 65% had a comorbid condition.
Those receiving the plasma derived no significant clinical benefit over placebo.
“At day 30 day, no significant difference was noted between the convalescent plasma group and the placebo group in the distribution of clinical outcomes according to the ordinal scale (odds ratio, 0.83; 95% confidence interval [CI], 0.52 to 1.35; P = 0.46),” the study authors wrote. “Overall mortality was 10.96% in the convalescent plasma group and 11.43% in the placebo group, for a risk difference of −0.46 percentage points (95% CI, −7.8 to 6.8).” Of note, the “total SARS-CoV-2 antibody titers tended to be higher in the convalescent plasma group at day 2 after the intervention.”
The study authors also pointed out that both groups had similar adverse or serious events.
“Our trial ensured that more than 95% of the transfused convalescent plasma units had a total anti–SARS-CoV-2 antibody titer of at least 1:800 and that the plasma volume infused had a correction factor according to the participant’s weight,” Simonovich and colleagues wrote. “This finding is in contrast to the findings of a series of non-randomized studies claiming convalescent plasma to be of substantial benefit and illustrates the importance of randomized, controlled trials, especially in the context of a pandemic.”
Simonovich and colleagues noted that they also had prespecified subgroup analyses in their trial “in an attempt to detect patient subpopulation for which previous reports had suggests that the use of convalescent plasma might have potential benefit.” Again, convalescent plasma struck out in both primary and secondary outcomes “including the 39 patients who received the intervention within 72 hours after the onset of symptoms,” they wrote. “We did find a difference in the primary outcome, in favor of placebo, for patients younger than 65 years of age (odds ratio 0.18; 95% CI, 0.06 to 0.54). Additional analysis of this subgroup failed to reveal any clear explanation, and we interpret this as a chance finding, although further confirmation in other studies may be warranted.”
The study authors cite several limitations of their trial, including the fact that all the patients had severe Covid-19 pneumonia, and the results may not be generalizable to other groups with milder disease. The time of disease onset to respiratory failure was similar to the time of symptom onset to trial enrollment (around 7 days) so it is not known if therapy started earlier might have had a different outcome. “Indeed, studies with specific antibodies administered within 72 hours of Covid-19 diagnosis in patients with risk factors for severe disease are currently ongoing or planned,” Simonovich and colleagues wrote.
- Convalescent plasma did not show benefit over placebo in the treatment of patients with severe Covid-19, according to the results of a double-blind, placebo-controlled trial.
- Overall mortality at day 30 was not significantly different between the convalescent plasma group and the placebo group.
Candace Hoffmann, Managing Editor, BreakingMED™
The study was supported by the participant institutions. The COVIDAR test for SARS-CoV-2 IgG was developed at Fundación Instituto Leloir, with funding from the National Council of Scientific Research and Technology (CONICET) Institute, National Ministry of Science, Technology, and Innovation of Argentina.
Cat ID: 254
Topic ID: 253,254,254,930,791,932,730,933,192,927,151,928,925,934