Having metabolic syndrome was a significant risk factor for acute respiratory distress syndrome (ARDS) and death among patients hospitalized with Covid-19, according to findings from a global prospective study involving 29,000 patients.
Patients with metabolic syndrome were more likely to be placed on mechanical ventilation or extracorporeal membrane oxygenation (ECMO) and require non-invasive ventilation or high-flow oxygen support and supplemental oxygen, compared to patients without the metabolic syndrome.
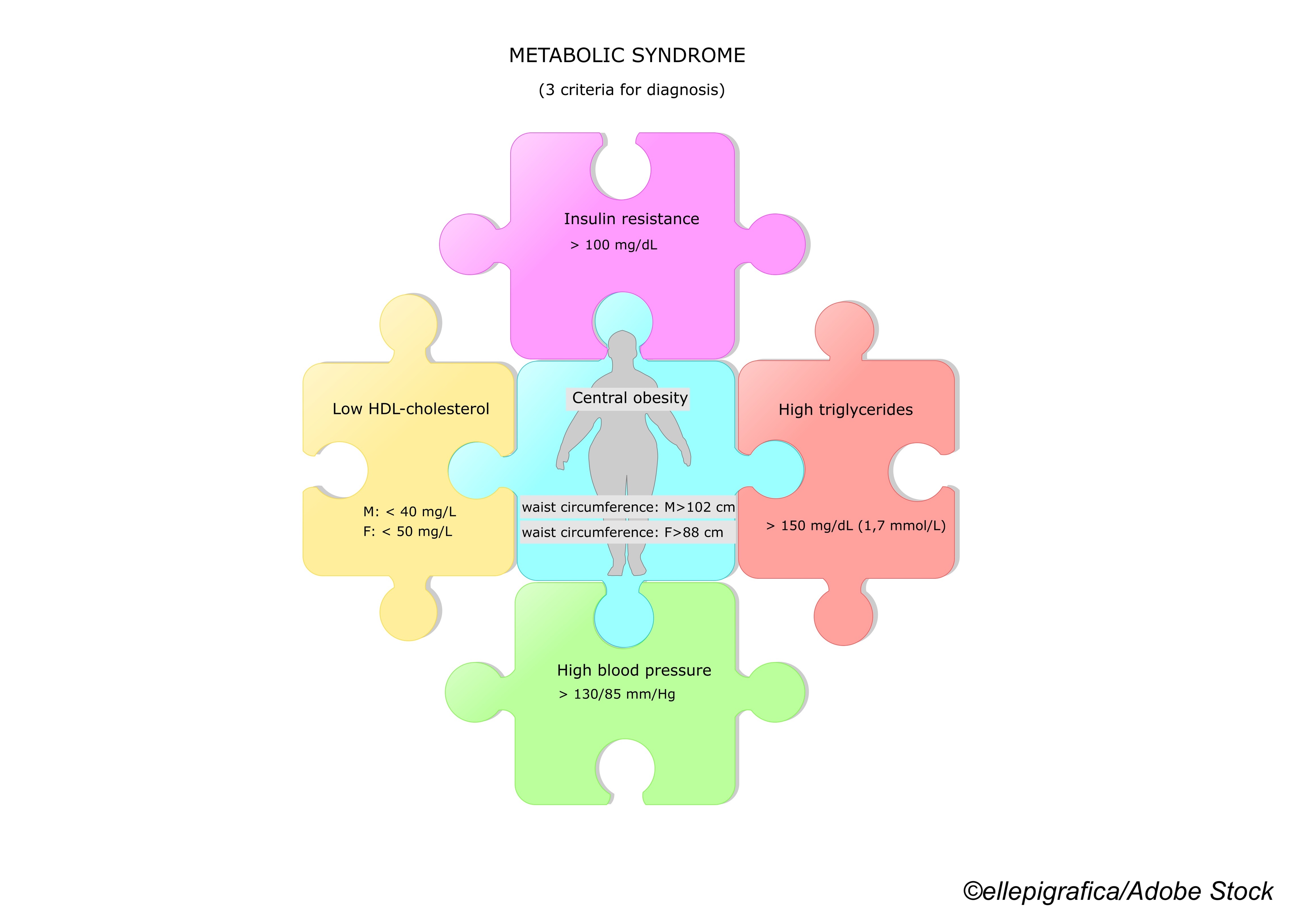
While the individual components of metabolic syndrome, including obesity, diabetes, hypertension, and dyslipidemia, have all been linked in earlier studies to poorer Covid-19 outcomes, the reasons for this are not fully understood, wrote researcher Joshua Denson, MD, of Tulane University School of Medicine, New Orleans, and colleagues.
“In smaller series, metabolic syndrome and its chronically low-grade inflammatory state has been postulated as instrumental in predisposing patients to ARDS and subsequently mortality,” the researchers wrote in JAMA Network Open. The study findings were published online Dec. 22.
“Our findings support this hypothesis, as patients with metabolic syndrome were not only at higher risk of ARDS and severe outcomes overall, but each additional metabolic syndrome criteria added was associated with greater risk of ARDS in an additive fashion among patients with one, two, three, or four metabolic syndrome criteria.”
They noted that metabolic syndrome is a chronic low-grade inflammatory state “characterized by subtly elevated acute-phase reactant levels, and endothelial dysfunction, which are also seen in Covid-19 and ARDS.”
The researchers analyzed data from the Society of Critical Care Medicine Discovery Covid-19 Viral Respiratory Illness Universal Study (VIRUS) international registry, which included patients treated for Covid-19 at 181 hospitals across 26 countries.
A total of 29,040 patients hospitalized for Covid-19 between mid-February 2020 and mid-February 2021 met eligibility criteria for the analysis. The study authors split the cohort into two groups: patients with metabolic syndrome—defined as the presence of three or more of the following: obesity; pre-diabetes or diabetes; hypertension; and dyslipidemia—and control participants who did not have metabolic syndrome.
The primary outcome was in-hospital mortality, and secondary outcomes included progression to ARDS, ICU admission, need for invasive mechanical ventilation, and hospital length of stay.
The average age of the hospitalized patients included in the analysis was 61 years, 45% were female, 23% were Black, 18% were Hispanic, and roughly 58% were White.
A total of 5,069 patients (17.5%) met the criteria for having metabolic syndrome, and these patients were compared with close to 24,000 control patients (82.5%) without metabolic syndrome.
Among the study’s main findings (adjusted analyses), those with metabolic syndrome had:
- An increased risk of ICU admission (adjusted odds ratio [aOR], 1.32; 95% CI, 1.14-1.53), invasive mechanical ventilation (aOR, 1.45; 95% CI, 1.28-1.65), ARDS (aOR, 1.36; 95%CI, 1.12-1.66), and mortality (aOR, 1.19; 95% CI, 1.08-1.31).
- Greater risk for prolonged hospital length of stay (median [IQR], 8.0 days versus 6.8 days; P<0.001) and ICU length of stay (median [IQR], 7.0 days versus 6.4 days; P<0.001).
“Each additional metabolic syndrome criterion was associated with increased cumulative risk of ARDS (one criterion: 1,147 patients with ARDS [10.4%]; P=0.83; two criteria: 1,191 patients with ARDS [15.3%]; P<0.001; three criteria: 817 patients with ARDS [19.3%]; P<0.001; four criteria: 203 patients with ARDS [24.3%]; P<0.001),” the study authors wrote.
Denson and colleagues noted that given the high rates of metabolic syndrome, along with obesity and diabetes, in the United States, “one hypothesis for why the U.S. led the world in Covid-19 cases and deaths could be the high prevalence of metabolic syndrome in this population.”
Study limitations cited by the researchers included the observational design of the study and the possibility that unmeasured confounders could have impacted the findings.
“Also, selection and information bias were considered important limitations owing to the unavailability of data from the electronic medical record. However, to mitigate this potential bias, several analyses were performed to support the statistical approach in addressing incomplete data,” they wrote.
The researchers concluded that the study showed “metabolic syndrome, diagnosed by the clustering of obesity, pre-diabetes or diabetes, hypertension, and dyslipidemia, was associated with significantly increased mortality and ARDS in a global population of hospitalized patients with Covid-19.”
“This increased risk was cumulative, with the proportion of ARDS increasing with each added metabolic syndrome criteria,” they added.
-
Having metabolic syndrome was a significant risk factor for acute respiratory distress syndrome (ARDS) and death among patients hospitalized with Covid-19 in a global prospective study involving 29,000 patients.
-
Patients with metabolic syndrome were more likely to be placed on mechanical ventilation or extracorporeal membrane oxygenation (ECMO) and require non-invasive ventilation or high-flow oxygen support and supplemental oxygen, compared to patients without metabolic syndrome.
Salynn Boyles, Contributing Writer, BreakingMED™
Funding for this research was provided y the American Diabetes Association Covid-19 Research Award, the Society of Critical Care Medicine, Janssen Research & Development, the U.S. National Institutes of Health and others. Denson reported receiving grants from the American Diabetes Association, SCCM, Gordon and Betty Moore Foundation, and NIH during the conduct of the study and personal fees from AstraZeneca, GlaxoSmithKline, Guidepoint Global Advisors, and Duke University outside the submitted work.
Cat ID: 125
Topic ID: 79,125,730,933,305,307,125,926,192,927,151,928,925,934