Racial disparity in medicine is not a new issue, but addressing it has taken on a new urgency in light of the national discussion of race triggered by the events of recent years, so it is not surprising that the National Kidney Foundation and the American Society of Nephrology named a task force to examine the use of race in the diagnosis and treatment of kidney disease.
In the United States, most labs calculate estimated glomerular filtration rate (eGFR) using a Black race coefficient in their calculations, but critics say that algorithm may lead to inaccurate GFR estimates for Black patients and may, in fact, contribute to worse clinical outcomes.
A pair of National Institute of Diabetes and Digestive and Kidney Diseases-supported trials examined the use of race in estimating GFR and came away with a similar, and somewhat surprising, conclusion: “equations based on cystatin C yielded lower predictive bias and greater agreement with measured GFR across race groups than GFR estimation based on creatinine alone. Moreover, they showed that bias and agreement were not affected by the inclusion of race as a predictor.”
That assessment comes from an editorial by a pair of New England Journal of Medicine deputy editors—Winfred W. Williams, MD, and Julie R. Ingelfinger, MD, and a NEJM statistician Joseph W. Hogan, SD.
In the first paper, Lesley A. Inker, MD, MS, Director of the Kidney and Blood Pressure Center, the Kidney Function and Evaluation Center, and Quality Improvement at Tufts University School of Medicine in Boston, and colleagues developed new eGFR equations “using data culled from 10 studies (n=8,254, 32.5% Black) for serum creatinine and 13 studies (n=5,352, 39.7% Black) for both serum creatinine and cystatin-C. They tested the accuracy of the new equation by comparing it to measured GFR in a validation data set (12 studies, n=4,050, 14.3% Black).
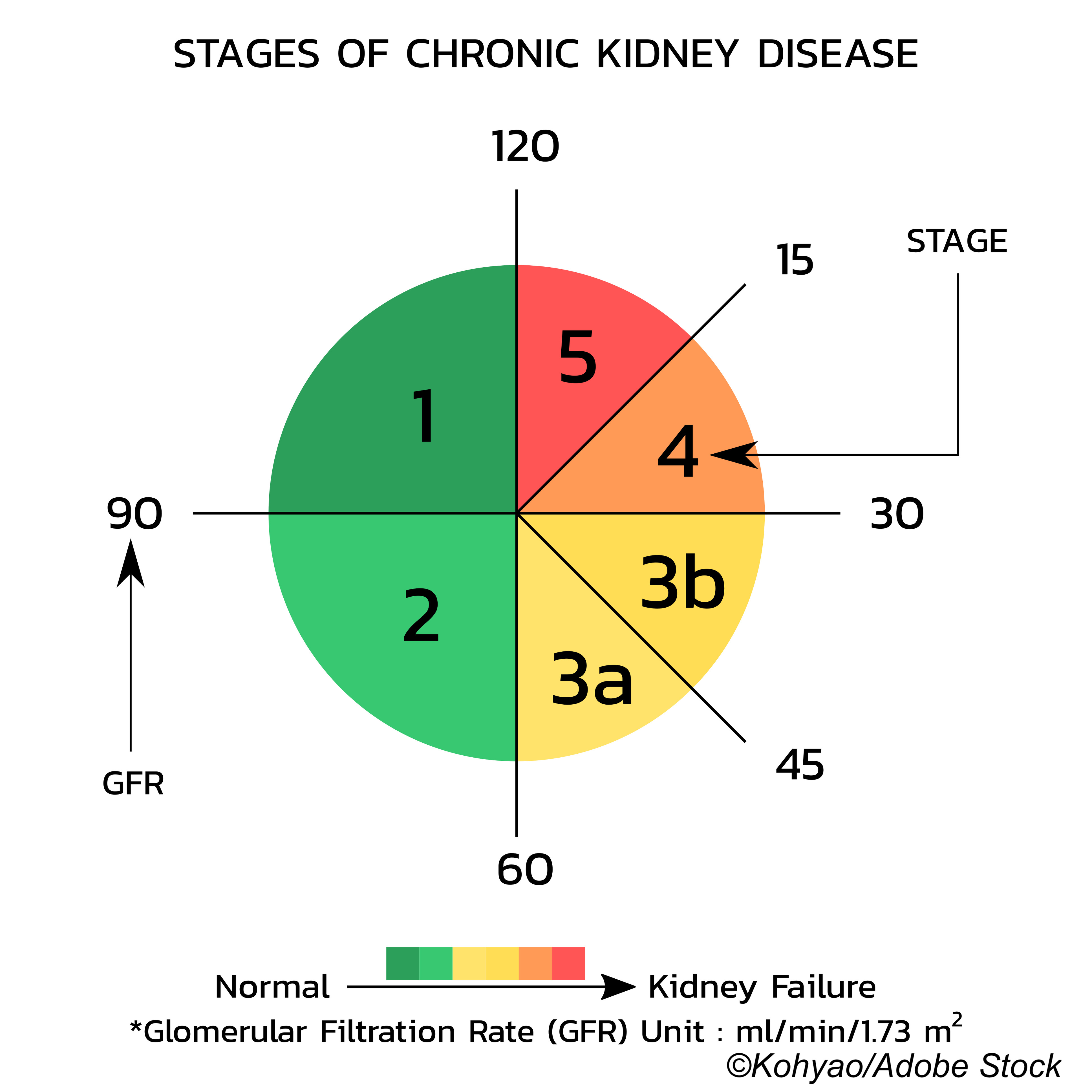
“We projected the prevalence of chronic kidney disease (CKD) and GFR stages in a sample of U.S. adults, using current and new equations… New creatinine–cystatin C equations without race were more accurate than new creatinine equations, with smaller differences between race groups. As compared with the current creatinine equation, the new creatinine equations, but not the new creatinine–cystatin C equations, increased population estimates of CKD prevalence among Blacks and yielded similar or lower prevalence among non-Blacks,” they wrote in The New England Journal of Medicine. “Because all equations were developed by the CKD-EPI research group, we refer to them only by the filtration marker or markers (creatinine [eGFRcr], cystatin C [eGFRcys], or creatinine–cystatin C [eGFRcr-cys]) and the demographic factors (age, sex, and race [ASR] or age and sex [AS]) that were used in their development.”
In the second paper, Chi-yuan Hsu, MD, of the University of California, San Francisco, and Kaiser Permanente Northern California in Oakland, and colleagues looked at a national study of adults with chronic kidney disease and conducted a cross-sectional analysis of baseline data—race, genetic ancestry markers, serum creatinine, serum cystatin C, and 24-hour urinary creatinine levels—from 1,248 of the study’s participants.
When Hsu and colleagues used current GFR estimating equations, they found that among those who identified as Black using a GFR equation model that omitting race resulted in “more underestimation of the GFR (median difference between measured and estimated GFR, 3.99 ml per minute per 1.73 m2 of body-surface area; 95% confidence interval [CI], 2.17 to 5.62) and lower accuracy (percent of estimated GFR within 10% of measured GFR [P10], 31%; 95% CI, 24 to 39) than models that included race (median difference, 1.11 ml per minute per 1.73 m2; 95% CI, −0.29 to 2.54; P10, 42%; 95% CI, 34 to 50).”
Likewise, incorporating genetic ancestry data resulted in similar results, they wrote. Moreover, including “non-GFR determinants of the serum creatinine level (e.g., body-composition metrics and urinary excretion of creatinine) that differed according to race reported by the participants and genetic ancestry did not eliminate the misclassification introduced by removing race (or ancestry) from serum creatinine–based GFR estimating equations.”
But including cystatin C in the GFR calculation could “achieve similarly statistically unbiased (median difference, 0.33 ml per minute per 1.73 m2; 95% CI, −1.43 to 1.92) and accurate (P10, 41%; 95% CI, 34 to 49) estimates in Black participants…”
Inker et al also warned that their analyses “show that the new eGFRcr(ASR-NB) equation, as has been adopted by some institutions, could lead to large errors in GFR estimation in some Black persons—for example, as Hsu et al. now report in the Journal. The new eGFRcr(AS) equation may be more equitable than the new eGFRcr(ASR-NB) equation because it averages observed differences across all persons and may be more appropriate for the increasingly diverse U.S. population. As compared with the ASR-NB equation, the AS equation decreases the bias in Black persons but also introduces a bias in non-Black persons; the magnitude of the bias in each group reflects the proportion of Black participants included in the development data set, which emphasizes the importance of including diverse populations in these data sets.”
In their editorial, Williams, Hogan, and Ingelfinger hammered home the fact that getting eGFR right is crucial diagnosis and management of kidney disease. “The use of the current CKD-EPI equations without application of the inflation factor for Black race (15.9% for the eGFRcr equation and 8.0% for the eGFRcr-cys equation) does not affect the accuracy of eGFR estimates for non-Black persons, but it underestimates the GFR and reduces accuracy for Black persons.”
In the real world of clinical practice, finding eGFR equations that don’t rely on racial adjustment has been difficult.
“Inker et al. found that, relative to the currently used 2009 CKD-EPI eGFRcr equation, the same equation refitted without race had a similar percent agreement between eGFR and measured GFR within CKD stages but retained modest statistical bias,” Williams et al wrote. “However, Hsu et al. found that in models of eGFR that were based on serum creatinine, exclusion of race-based predictors (i.e., Black race as reported by the participants or percentage of African ancestry) yielded increased predictive bias and diminished accuracy; furthermore, the effect of excluding race as a predictor could not be mitigated by replacing race with non-GFR determinants of the serum creatinine concentration. In contrast, race had no effect on the predictive accuracy of eGFR in equations that were based on cystatin C. Both articles point to the promise of cystatin C for uniformly more accurate GFR prediction without the need to include race-based adjustments.”
Against this background, the report issued by the NKF-ASN task force is takes a decidedly urgent stance in calling for:
- Immediate implementation of the CKD-EPI creatinine equation refit without the race variable in all laboratories.
- A national effort to facilitate “increased, routine, and timely use of cystatin C, especially to confirm eGFR in adults for clinical decision-making.”
- Research on GFR estimation with new endogenous filtration markers.
That action is needed is hardly surprising since, as the editorial writers point out:
“Meaningful ways to alleviate health care inequities are overdue. That Black persons with CKD often lose kidney function more rapidly and have lower kidney transplantation rates than patients from other racial and ethnic groups indicates an urgent problem. The use of the most accurate estimates of GFR may permit earlier identification and care of persons at risk.Irrespective of the equations adopted, estimates of GFR are, by their very nature, imperfect. Some promising options will take time to implement, since measurement of cystatin C is currently neither routine nor uniform. Both existing and newly derived equations have strengths and weaknesses, and change inevitably induces unanticipated consequences. Most important, however, is that estimates do no harm but rather help us care for all patients equally.”
-
Two studies that investigated the predictive value of eGFR equations when race was eliminated as an adjustment found that equations that factored in cystatin C as a variable more closely matched measured GFR.
-
Be aware that Black persons with CKD lose kidney function faster than non-Blacks and are less likely to receive transplants.
Peggy Peck, Editor-in-Chief, BreakingMED™
Both studies were funded by the National Institute of Diabetes and Digestive and Kidney Disorders.
Inker had no disclosures.
Hsu had no disclosures.
Williams, Hogan, and Ingelfinger are employed by The New England Journal of Medicine.
Cat ID: 127
Topic ID: 81,127,730,914,12,187,127,411,192,669,918,925