“Among adults with symptomatic chronic subdural hematoma, most of whom had undergone surgery to remove their hematomas during the index admission, treatment with dexamethasone resulted in fewer favorable outcomes and more adverse events than placebo at 6 months, but fewer repeat operations were performed in the dexamethasone group,” wrote Peter Hutchinson, PhD, of the University of Cambridge in England, and co-authors, in New England Journal of Medicine.
Within 72 hours of admission to a neurosurgical unit, patients with symptomatic chronic subdural hematoma received either a 2-week tapering course of oral (or nasogastric) dexamethasone starting at 8 mg twice daily, or placebo. The primary outcome was a modified Rankin score (mRS) at 6 months of 0-3, representing a favorable outcome (mRS ranges from 0=no symptoms to 6=death).
At admission, 60% of both groups had mRS of 1-3. Of 748 patients randomized, 94% had surgical treatment at the treating physician’s discretion.
Of 680 patients remaining with data at 6 months, a 0-3 mRS was seen in 87% overall, in 83.9% of the dexamethasone group and in 90.3% for placebo (difference −6.4 percentage points favoring placebo, 95% CI −11.4 to −1.4; P=0.01).
Repeat surgery for recurrence of the hematoma was performed on 1.7% in the dexamethasone group and 7.1% in the placebo group.
“Although the between group difference of 6.4 percentage points was below the 8 percentage-point difference used in the power calculation, this difference may be clinically relevant and may suggest harm associated with dexamethasone with regard to a favorable outcome on the modified Rankin scale,” the researchers noted.
“The beneficial effects of glucocorticoids in shrinking chronic subdural hematomas have long been intimated at,” noted Allan Ropper, MD, deputy editor of New England Journal of Medicine, in an accompanying editorial.
“Although the trial answers an important question that has lingered for 50 years by showing no benefit of glucocorticoids with respect to the disability outcome, it is perhaps less certain on the issue of whether glucocorticoids shrink the subdural collection and reduce the need for reoperations,” Ropper wrote. “The results of this trial reduce the enthusiasm for treating chronic subdural hematomas with glucocorticoids.”
“In the end, the lower percentage of patients who had a favorable disability outcome and the occurrence of more adverse events in the dexamethasone group tip the scale against using the drug,” he added.
A 2015 study of military and civilian populations projected that with rising incidence, chronic SDH would become the most common cranial neurosurgical condition in adults by 2030. The standard treatment is surgical evacuation for most patients.
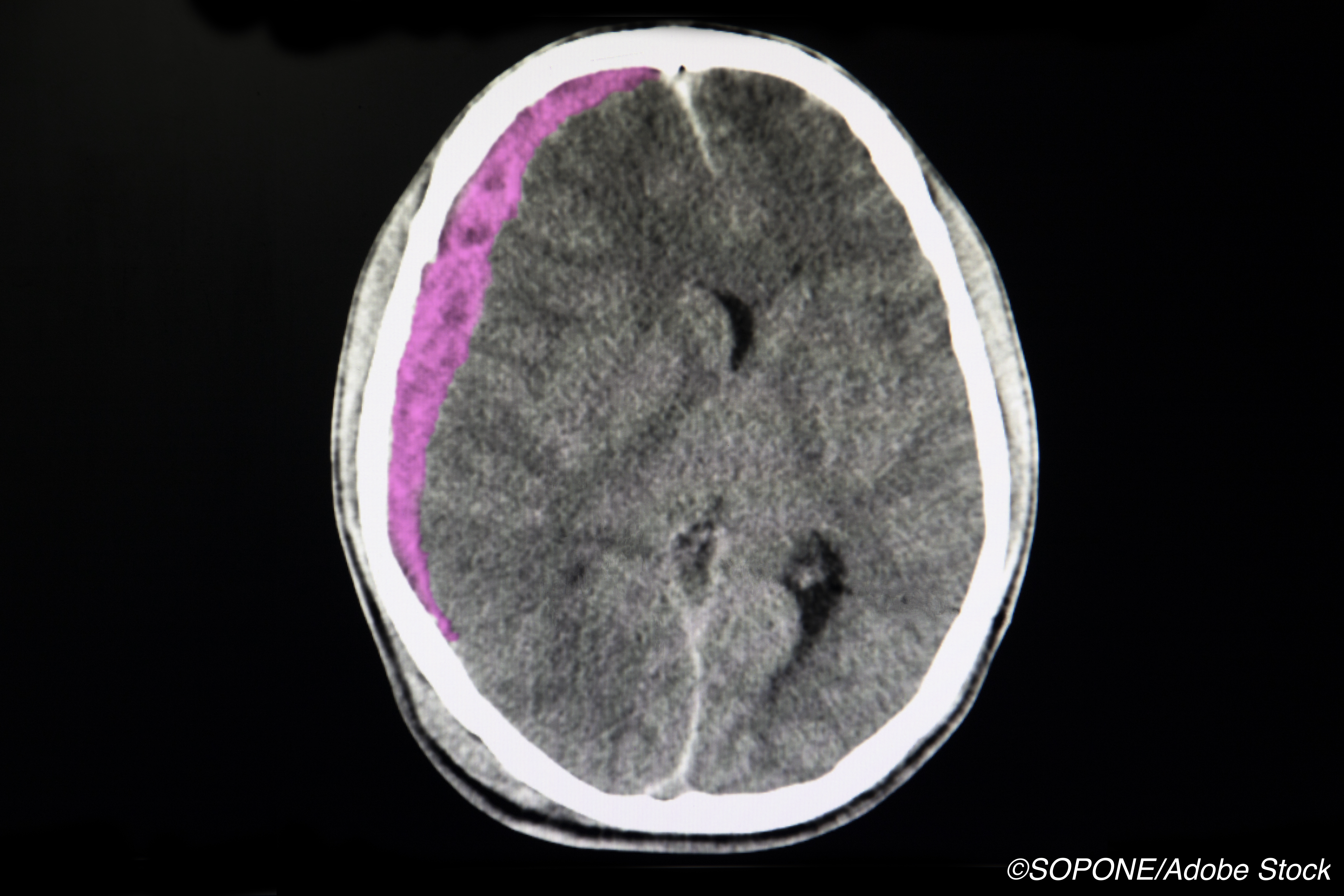
Chronic subdural hematoma is a membrane-bound collection of blood and fluid with inflammatory cells in the intracranial subdural space. It may occur with even minor or unnoticed trauma and presents with weakness, change in consciousness or cognition, headache, or gait disturbance. Hypodensity is seen on CT, rather than hyperdensity, which is seen with acute SDH.
The SDH lesion changes through processes of angiogenesis, fibrinolysis, and inflammation, and anti-inflammatory and anti-edematous properties of steroids have long been posited as an adjunct or stand-alone treatment that might improve outcomes or even eliminate the need for surgery.
A 2019 meta-analysis that addressed the ongoing debate about the role of corticosteroids in this setting included seven studies with high risk of bias. It concluded that “the addition of corticosteroids to surgery might be effective in the treatment of chronic SDH,” and stressed a need for randomized trials.
Hutchinson and colleagues analyzed data from patients enrolled in the Dex-CSDH trial between August 2015 and November 2019, randomizing 748 adult patients (375 to dexamethasone, 373 to placebo). Dexamethasone was given twice daily for 3 days each in doses of 8, 6, 4, and 2 mg, then once daily at 2 mg for 2 days.
Mean age of patients was 74 and about 72% of the dexamethasone and 77% of the placebo group were male. Known head trauma was present for 68% of the dexamethasone and 72% of the placebo groups, while any antithrombotic medication was used by 48% of the dexamethasone and 45% of the placebo groups.
Modified intention-to-treat analysis excluded patients who withdrew consent or who were lost to follow-up, leaving 680 patients (341 and 339 patients in the dexamethasone and placebo groups, respectively).
For 38 patients who did not have surgical evacuation of the hematoma, favorable outcome was reported in 18 of 22 patients (82%) in the dexamethasone group and in 16 of 16 patients (100%) in the placebo group. “Because almost all the patients underwent an initial operation to remove the hematoma, no firm conclusions could be drawn regarding the effect of dexamethasone as a method of conservative management to avoid surgery,” the researchers said.
Adverse events were more common in the dexamethasone group. Adverse events of special interest included hyperglycemia leading to treatment or discontinuation of the trial regimen, new-onset diabetes, hyperosmolar hyperglycemic state, new-onset psychosis, peptic ulceration or gastrointestinal bleeding, and other upper gastrointestinal side effects. They occurred in 41 patients (10.9%) in the dexamethasone group and 12 (3.2%) patients in the placebo group (OR 3.4, 95% CI 1.81-6.85)
Among events of special interest, those judged to be serious occurred in 16.0% of the dexamethasone group and 6.4% for placebo (OR 2.49, 95% CI 1.54-4.15).
Limitations included a 9% loss to follow-up by 6 months. In addition, patients and caregivers familiar with steroid effects may have become non-blinded during the trial.
-
Dexamethasone treatment for chronic symptomatic subdural hematoma led to fewer favorable outcomes than placebo, despite being associated with fewer repeat operations, a randomized trial found.
-
At 6 months, 83.9% of patients randomized to dexamethasone had a modified Rankin score of 0 to 3, representing a favorable outcome, compared with 90.3% for placebo.
Paul Smyth, MD, Contributing Writer, BreakingMED™
This study was supported by the National Institute for Health Research (NIHR) Health Technology Assessment Programme.
Hutchinson reported no disclosures.
Ropper is employed by the New England Journal of Medicine as Deputy Editor.
Cat ID: 130
Topic ID: 82,130,728,791,730,130,192,925,493


