Is primary resection with anastomosis and proximal diversion (PAPD) a viable alternative to the standard Hartmann procedure (HP) for Hinchey stage III or IV diverticular disease?
According to a retrospective, cross-sectional study, while HP is still the standard of care, PAPD produced similar outcomes, although PAPD was found to be associated with significantly increased readmission and ostomy rates. What’s more, the choice of HP or PAPD may come down to patient selection, as PAPD appears to favor younger, healthier patients.
The analysis from Yas Sanaiha, MD, Cardiac Outcomes Research Laboratory, University of California, Los Angeles, and colleagues, reviewed data from the Nationwide Readmissions Database of more than a million adults hospitalized for acute colonic diverticulitus and assessed those requiring non-elective HP or PAPD.
“Among 1,772 patients who underwent PAPD and survived index hospitalization, there was an increased incidence of 90-day readmission compared with 30,851 patients who underwent HP and survived index hospitalization (393 patients [22.2%] versus 4384 patients [14.2%]; P<0.001) with increased hazard of ostomy reversal (hazard ratio, 1.46; 95% CI, 1.08-1.99),” they wrote in JAMA Network Open.
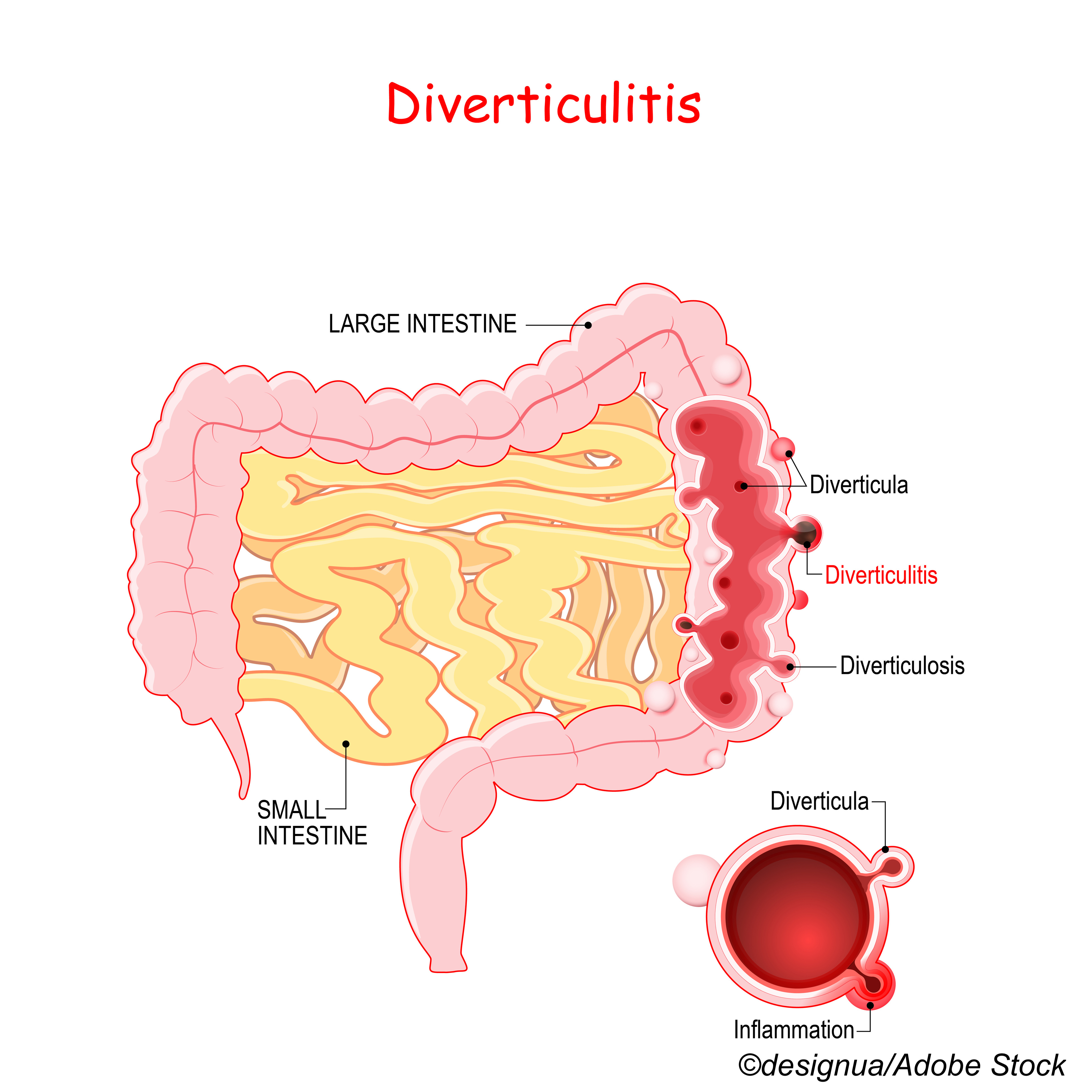
Writing in a commentary accompanying the study, Maryam K. Mohammed, MD, from the Department of Surgery, University of Pittsburgh Medical Center, Pennsylvania, and colleagues noted that diverticular disease is not only present in more than 50% of adults in the U.S. by age 70 but also costly at about $5.5 billion annually. The disease is usually not treated with surgery, even with perforation; however, “the presence of purulent or feculent peritonitis (Hinchey stage III or IV disease) warrants emergent operative intervention.”
Mohammed and colleagues noted that HP has been used for half a century “but is associated with decreased stoma reversal rates secondary to the morbidity associated with reversal of an end colostomy and colorectal anastomosis.”
Enter PAPD in the late 20th century, but uptake has been slow, the editorialists noted, “widely given lack of equipoise. In light of increasing evidence from retrospective analyses and randomized clinical trials (RCTs) finding equivalent rates of postoperative mortality and major complications with increased rates of stoma reversal after PAPD compared with HP, PAPD was included as a valid treatment option in clinical practice guidelines from the American Society of Colon and Rectal Surgeons (ASCRS) in 2014. Patients are often considered candidates for PAPD if proximal and distal ends of the colon are not inflamed and are amenable to anastomosis, the patient is not in septic shock, and the patient is not immunocompromised.”
But even now, PAPD is not widely used, as shown in Sanaiha and colleagues’ large retrospective analysis looking at data from 2014 to 2017. They found that there were 34,126 patients that needed diversion. Of those, 32,326 (94.7%) underwent HP, while just 1,800 (5.3%) underwent PAPD within 48 hours of hospital admission. However, the rate of PAPD use did increase over the study period from 2.6% to 7.1%.
Notably, “compared with patients undergoing HP, patients undergoing PAPD were younger (median [IQR] age, 60 [51-70] years versus 65 [54-74] years; P<0.001) and had decreased rates of comorbidities, including heart failure, coronary artery disease, and chronic pulmonary obstructive disease, demonstrating an overall lower risk profile,” the study authors noted. “Furthermore, patients undergoing PAPD had lower rates of multiorgan dysfunction (520 patients [28.9%] versus 11,514 patients [35.6%]; P<0.001), coagulopathy, and peritonitis. The prevalence of diabetes and chronic liver disease was similar across the 2 operative strategies. Although there was no statistically significant difference in income distribution between groups, individuals in the PAPD group were more commonly privately insured.”
Among their other findings comparing HP to PAPD, respectively:
- Index mortality: 1,475 (4.6%) versus 28 (1.5%).
- Composite complication: 14,348 (44.4%) versus 634 (35.2%).
- 30,851 versus 1,772 survived index hospitalization.
- Non-home discharge: 8,394 (27.3%) versus 332 (18.8%).
- 30-day readmission: 3,415 (11.1%) versus 336 (19.0%).
- 31 to 90-day readmission: 1451 (4.7%) versus 122 (6.9%).
- Ostomy closure: 5983 (19.4%) versus 315 (17.8%).
“While there was no statistically significant difference in index outcomes, PAPD was associated with an increased risk-adjusted hazard of unplanned readmissions (hazard ratio [HR], 1.79; 95%CI, 1.44-2.23), with an increased rate of patients who underwent PAPD compared with those who underwent HP readmitted at least twice within the remainder of the calendar year (497 of 2,003 patients [24.8%] versus 4471 of 30,330 patients [14.7%]; P<0.001),” the study authors wrote.
The study authors also looked at the overall costs of PAPD versus HP, which “were comparable for the remainder of the year ($87,484 [$57,979-$142,394] versus $87,084 [$55,508-$142,638]; P=.87) but median (IQR) total hospitalization days were not (13 [10-20] days versus 15 [12-22] days; P<0.001),” they wrote. “However, median (IQR) cost for the first readmission episode within 30 days of discharge was increased for patients undergoing HP ($13,428 [$8962-$19,623] vs $8,500 [$5,996-$12,589]; P<0.001). Counterfactual modeling suggested that were all patients who underwent HP readmitted at the rate of patients who underwent PAPD within one month of discharge, readmission costs would increase by $3.7 million at the national level.”
Insurance coverage appeared to favor PAPD over HP. The study authors also found that there were similar rates of PAPD at teaching and non-teaching hospitals, although they noted that this finding “may be associated with practice changes in response to society guidelines that have led to expansion of this surgical technique beyond academic settings.”
Patient selection for either surgical intervention is key, Sanaiha and colleagues noted. “Furthermore, the association between age and acuity may result in similar patient severity in an older patient with decreased physiologic reserve and a younger patient with delayed presentation. Surgeons have achieved comparable outcomes with use of PAPD through rigorous patient selection. Taken together, our results suggest a cautious approach to routine adoption of PAPD in practice guidelines.”
Mohammed and colleagues agreed: “While the results of this and antecedent studies suggest that PAPD can likely be used more widely, favorable outcomes associated with PAPD may be greatly dependent on judicious preoperative risk assessment, patient selection, and surgeon experience or comfort. Perhaps these data also suggest that primary resection and anastomosis without proximal diversion should be considered among patients for whom HP is not indicated, given the frequency of stomal complications and paucity of anastomotic complications in this population. Risk factors, patients’ goals and values, and intraoperative findings should all be considered when choosing operative procedure. We believe that primary resection and anastomosis should be used with increasing frequency, but we strongly oppose the notion that HP should be considered a procedure of antiquity.”
The authors noted several limitations of their study, including its non-randomized design and that nutritional parameters and duration of symptoms were not available.
“Furthermore, changes in administrative coding schema from ICD-9 to ICD-10 in 2015 limit the interpretation of our trend analysis, particularly the magnitude of increase in PAPD performance,” they noted.
-
Although the Hartmann procedure (HP) is still the standard of care for Hinchey stage III or IV diverticular disease, primary resection with anastomosis and proximal diversion (PAPD) produced similar outcomes; however, PAPD was found to be associated with significantly increased readmission and ostomy rates.
-
PAPD appears to be a viable option for younger, healthier patients.
Candace Hoffmann, Managing Editor, BreakingMED™
None of the authors cited in this article disclosed any relevant relationships.
Cat ID: 23
Topic ID: 78,23,730,188,23,192,925,159