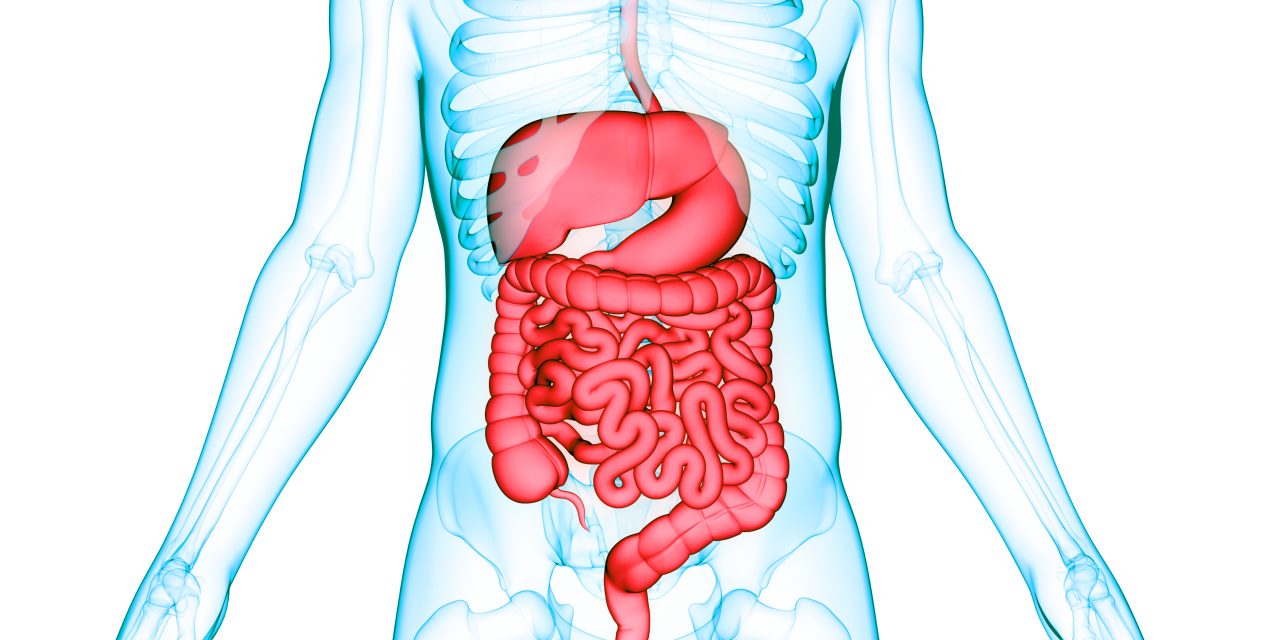
Ileocolonoscopy remains the mainstay of objective disease assessment in Crohn’s Disease, and various validated indices are used to grade severity of the disease. The most commonly used indices are the Simple Endoscopic Score for Crohn’s Disease (including the size of ulcers) and the Crohn’s Disease Endoscopic Index of Severity (including the depth of ulcers). These measurements are highly subjective, especially the depth of an ulcer, and are based solely on the discretion of the endoscopist coupled with the imaging capabilities of the colonoscope and adequacy of the bowel prep. Narula et al. undertook a post hoc analysis of baseline predictors of endoscopic remission (ER) at week 26 in a subset (172 of 508) of moderate-severe Crohn’s disease patients participating in the SONIC trial. The authors found no significant differences in the odds of achieving ER when comparing overall or segmental severe inflammation (high Simple Endoscopic Score for Crohn’s Disease [>16 overall or >3 per segment] or Crohn’s Disease Endoscopic Index of Severity [>12 overall or >3 per segment] scores) with moderate inflammation. The number of affected segments involved also did not impact the likelihood of achieving week 26 ER. The authors then found a potentially synergistic effect with large and deep ulcers in the ileum and rectum. The optimal time to assess whether ulcers ultimately heal or not is unknown, but waiting longer than 26 weeks may negate any lead time bias regarding ulcer size. Therefore, similar to many areas of life, it is likely that size ultimately does not matter, but instead location, location, and location.
Does Size Really Matter?