1. In a large Swedish cohort of singleton births following the use of assisted reproductive technology, double embryo transfer was associated with significantly higher odds of neonatal death compared to single embryo transfer.
2. Both double and single embryo transfers were associated with an increased risk of congenital malformations compared to singleton births conceived without assistive reproductive technology.
Evidence Rating Level: 2 (Good)
Study Rundown: Conception via assisted reproductive technology has been linked to both obstetric risks and higher rates of neonatal complications, often linked to multiple gestations. This study aimed to assess whether the transfer of multiple embryos plays a significant role in this risk by comparing singleton births after single embryo transfer to double embryo transfer. Among about 31,000 births after single embryo transfer and 5,000 after double embryo transfer, the adjusted risk of neonatal death was higher in the double embryo transfer group at 0.3% compared to 0.1% in the single embryo group, indicating a significantly increased risk of neonatal death at an odds ratio of 2.67. Double embryo transfer was associated with a higher risk of low birth weight in the subgroups of frozen, but not fresh, cycles as well as transfers at the blastocyst, but not cleavage, stage. Compared to births following non-assisted conception within the same database, both single and double embryo transfer were associated with a higher risk of congenital malformations, but only double embryo transfer was associated with a higher risk of neonatal death. This large cohort study supports the notion that there are increased rates of neonatal morbidity and mortality in double embryo compared to single embryo transfer, although other factors such as fresh or frozen embryo status modified the effect. Although models were adjusted for factors that might motivate patients and providers to opt for double embryo transfer, including increased maternal age and history of spontaneous abortions, residual confounding due to differences in fertility potential may account for some part of the differences between the single and double embryo transfer groups.
Click to read the study in JAMA Pediatrics
Relevant Reading: Neonatal and maternal outcome after frozen embryo transfer: Increased risks in programmed cycles
In-Depth [retrospective cohort]: Live singleton births in Sweden between 2007 and 2017 were included. Data were drawn from a national assisted reproduction database and birth register. Infants with diagnosed genetic or chromosomal abnormalities were excluded. Both fresh and frozen embryo transfers at either cleavage or blastocyst stage were included. Odds ratios and relative risk ratios were estimated using logistic regression after adjustment for maternal age, birth order, delivery year, maternal birth country, previous spontaneous abortions, extrauterine pregnancies, and number of stimulation cycles. The 95% confidence interval (CI) for the risk of neonatal death in double compared to single embryo transfers was 1.28 to 5.55. This significant association persisted in a sensitivity analysis excluding possible multiple gestations, or vanishing twin syndrome. Within the frozen embryo subgroup, the risk of low birth weight was 5.4% for double embryo transfers versus 3.3% for single, yielding a relative risk ratio of 1.64 (95% CI 1.19-2.25). For blastocyst transfers, the respective rates of low birth weight were 7.4% and 4.2%, and the relative risk ratio was 1.83 (95% CI 1.29-2.60).
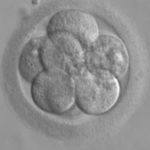
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.