The following is a summary of “Cognitive and Clinical Characteristics of Patients With Limbic-Predominant Age-Related TDP-43 Encephalopathy,” published in the May 2023 issue of Neurology by Pagnotti, et al.
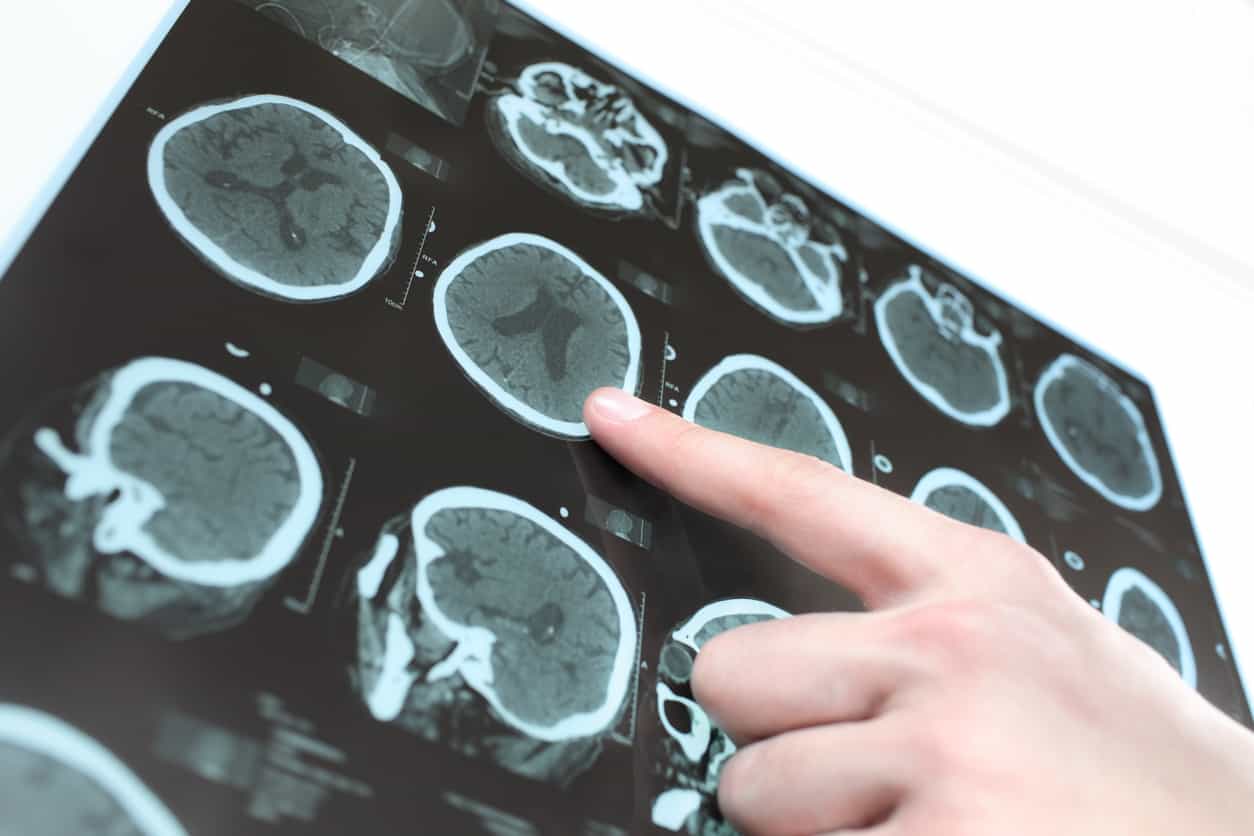
Limbic-predominant age-related TDP-43 encephalopathy (LATE) shares neuroanatomical networks with Alzheimer’s disease (AD) and is often comorbid with AD but is frequently missed in clinical diagnosis. For a study, researchers sought to identify baseline clinical and cognitive differences between patients with autopsy-confirmed LATE, AD, and comorbid LATE + AD.
The National Alzheimer Coordination Center provided clinical and neuropathologic datasets. Baseline data from individuals over 75 years old, without frontotemporal lobar degeneration, were included. Pathologically defined groups representing LATE, AD, and LATE + AD were analyzed. Group differences in clinical characteristics and cognition were assessed using analysis of variance and the χ2 test, utilizing measures from the Uniform Data Set.
The pathology groups consisted of 31 individuals with LATE (mean age: 80.6 ± 5.4 years), 393 with AD (mean age: 77.8 ± 6.4 years), and 262 with LATE + AD (mean age: 77.8 ± 6.6 years), with no significant differences in sex, education, or race. Participants with LATE pathology had a significantly longer lifespan (mean visits: LATE = 7.3 ± 3.7; AD = 5.8 ± 3.0; and LATE + AD = 5.8 ± 3.0; F(2,683) = 3.7, P < 0.05), reported later onset of cognitive decline (mean onset: LATE = 78.8 ± 5.7; AD = 72.5 ± 7.0; and LATE + AD = 72.9 ± 7.0; F(2,516) = 6.2, P < 0.01), and were more likely to be diagnosed as cognitively normal at baseline (LATE = 41.9%; AD = 25.4%; and LATE + AD = 12%; χ2 = 38.7, P < 0.001). In addition, participants with LATE (45.2%) reported fewer memory complaints compared to AD (74.4%) or LATE + AD (66.4%; χ2 = 13.3, P = 0.001) and were less likely to be classified as impaired on the Mini-Mental State Examination (LATE = 6.5%; AD = 24.2%; and LATE + AD = 40.1%; χ2 = 29.20, P < 0.001). Participants with LATE + AD pathology performed significantly worse than the AD and LATE groups across all neuropsychological measures.
Individuals with LATE pathology experienced cognitive symptoms at a later age and had a longer lifespan compared to those with AD or LATE + AD pathology. They were more likely to be classified as “cognitively normal” based on objective screening and self-report measures and performed better on neuropsychological testing. Comorbid pathologies resulted in more significant cognitive and functional impairment. The clinical presentation alone was insufficient to differentiate LATE from AD, underscoring the need for a validated biomarker.