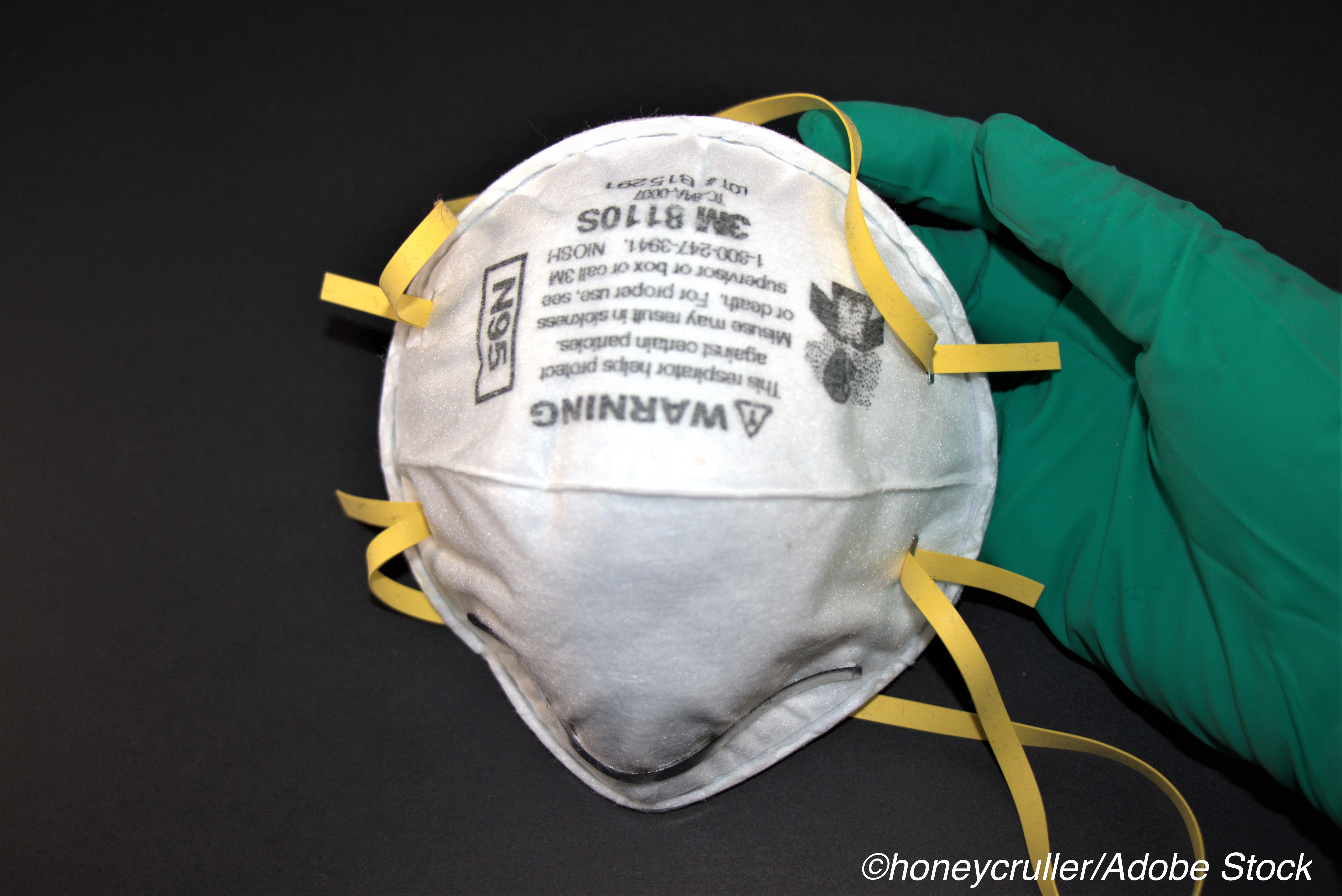
Expired N95 respirators, including those that have been used and sterilized, are acceptable alternatives to protect clinicians and other health care workers during the Covid-19 pandemic when new N95 respirators are unavailable, researchers found.
According to a study assessing face mask alternatives for potential use during the pandemic, the researchers determined that expired N95 masks with intact elastic straps, and used-sterilized respirators, had fitted filtration efficiencies (FFEs) of more than 95%, which is comparable to the face mask ratings for new N95 masks.
The study, by Emily E. Sickbert-Bennett, MS, PhD, UNC Health Care, Chapel Hill, North Carolina, and colleagues, was published in JAMA Internal Medicine.
When the Covid-19 pandemic hit many clinicians and healthcare workers faced shortages of personal protective equipment, particularly filtering face-piece respirators. This resulted in the need to find alternatives when National Institute for Occupational Safety and Health (NIOSH)-approved respirators are not available.
In this study, Sickbert-Bennett and colleagues assessed the FFEs of face mask alternatives used during the pandemic, including expired N95 respirators, N95 respirators that have been sterilized, CDC-approved imported respirators, respirators not listed as approved, and surgical or procedure masks with ties and ear loops.
Sickbert-Bennett and colleagues conducted fitted filtration efficiency tests on 29 face mask alternatives (on 1 man and 1 woman) between April and June 2020. They found that the most effective face mask was the Controlled Air Purifying Respirator system (MAXAIR) fitted with a face shield, which prevented 99% of particles from entering the test individual’s breathing space.
N95 respirators that were as many as 11 years past their expiration, and N95 respirators subjected to ethylene oxide and vaporized hydrogen peroxide sterilization had FFEs that remained above 95%.
All of the respirators not listed as approved failed to achieve 95% FFE, including:
- SAS Safetycorp 8617 Duckbill (93.2%).
- Fangtian Duckbill FT-032 with exhaust valve (86.2%).
- Safe-Life N95 B150 (85.9%).
- Jia Hu Kang KN95 mask with ear loops (85.1%).
- Zhongshan Dongfeng Huangshang GM700 (79.2%).
- Guangdong Fei Fan K95 (53.2%).
The CDC-approved, imported, non–NIOSH-approved respirators (the Dasheng DTC-3X-1 and Dasheng DTC-3X-2) also failed to achieve 95% FFE (79.7% and 76.8%, respectively).
In addition, the authors found that surgical and procedural masks secured with either ties or ear loops also had lower filtration efficiency, with those secured with elastic ear loops showing the lowest efficiency (38.1% overall FFE) of all masks tested.
As for the comparison of effectiveness between a man and a woman, the authors found that while the small 1860 N95 respirator (3M) on the man and the regular 1860 N95 respirator on the woman did not surpass FFEs of 95%, both were more than 90% efficient. All of the other single-sized N95 face masks were more than 95% efficient for both the man and woman
“[T]he CDC and Infectious Diseases Society of America has recommended the use of N95 respirators especially during aerosol-generating procedures as long as the supplies are available,” Sickbert-Bennett and colleagues concluded. “This evaluation provides quantitative results on which health care administrators, supply chain leaders, and hospital epidemiologists can make evidence-based decisions to protect clinicians and other health care workers during a pandemic or long-term mask shortage.”
In a commentary accompanying the study, Caitlin M. Dugdale, MD; Rochelle P. Walensky, MD, MPH, both of the Division of Infectious Diseases, Department of Medicine, Massachusetts General Hospital, and Harvard Medical School, Boston, Massachusetts, said the performance of these nonstandard approaches to preserving the N95 mask supply, as demonstrated by Sickbert-Bennett and colleagues, is “reassuring.”
Dugdale and Walensky also suggested that despite the less than perfect filtration efficiency of non-NIOSH approved respirators and surgical masks as demonstrated in the laboratory, “there is reason for optimism regarding their real world effectiveness.”
According to Dugdale and Walensky, no documented SARS-CoV-2 outbreaks have been linked to settings in which surgical masks were diligently used instead of N95 masks, “which suggests that even if airborne transmission is a considerable contributor to SARS-CoV-2 transmission, surgical masks are likely sufficient to prevent it.”
-
Expired N95 masks with intact elastic straps, as well as those that have been used and sterilized, are appropriate alternatives for healthcare workers when new N95 masks are unavailable.
-
All of the respirators not listed as approved by the CDC or National Institute for Occupational Safety and Health and evaluated in this study failed to achieve 95% filtration efficiency.
Michael Bassett, Contributing Writer, BreakingMED™
Sickbert-Bennett reports receiving consultation fees from PDI and Johnson & Johnson.
Dugdale reports receiving travel reimbursement from the Infectious Diseases Society of America and personal fees from the Joint United Nations Programme on HIV/AIDS.
Cat ID: 190
Topic ID: 79,190,254,930,791,932,730,933,190,926,192,927,151,928,925,934