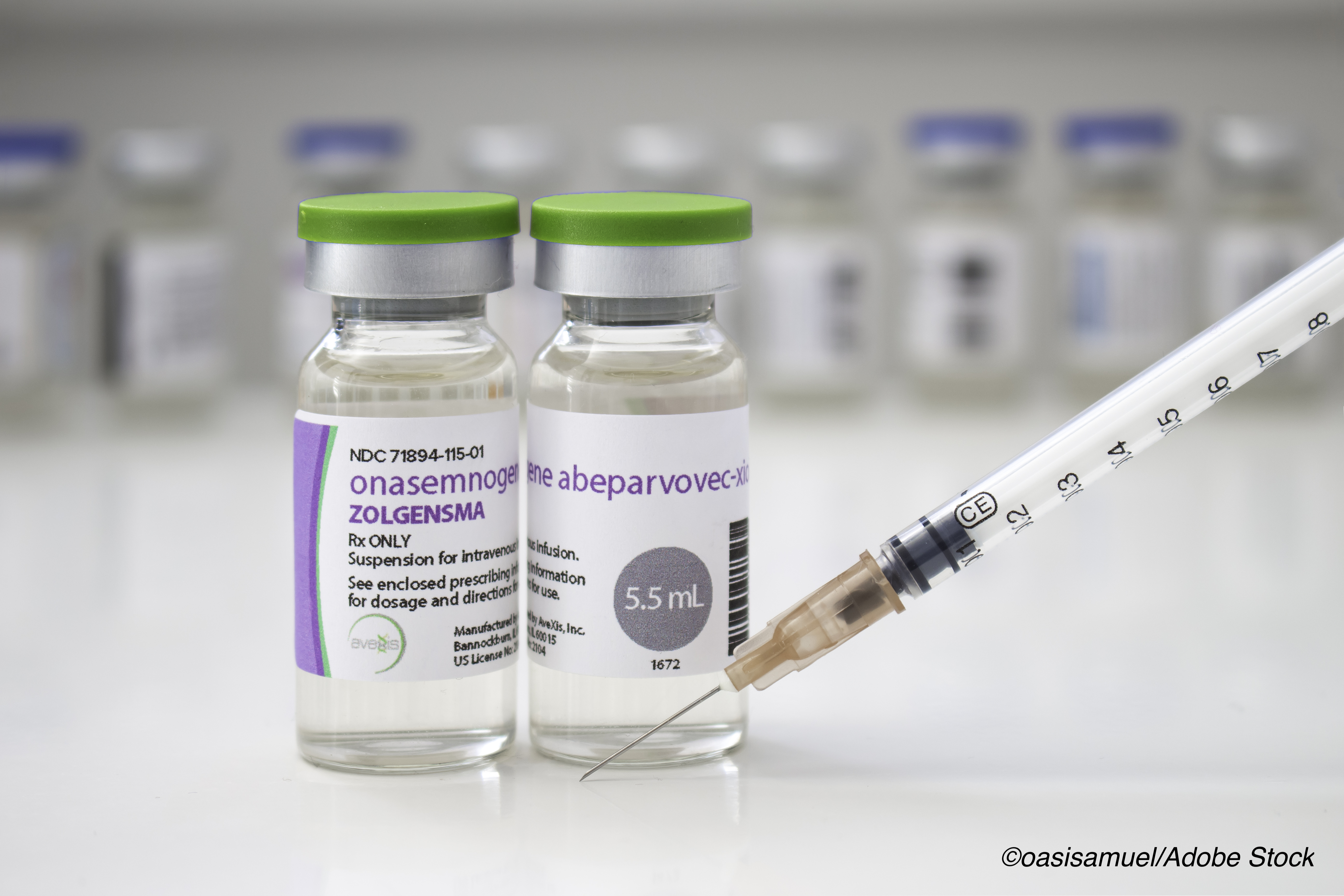
Onasemnogene abeparvovec gene therapy for spinal muscular atrophy (SMA) led to improvements in sitting and survival for infants with the most severe form of SMA, the phase III STR1VE trial found.
“In addition to better than expected survival, more than half of patients given onasemnogene abeparvovec reached the other primary endpoint of independent sitting at the 18 months of age study visit,” reported John Day, MD, of Stanford University in Palo Alto, California, and co-authors in Lancet Neurology.
“The favorable benefit–risk profile shown in this study supports the use of onasemnogene abeparvovec for treatment of symptomatic patients with genetic or clinical characteristics predictive of infantile-onset spinal muscular atrophy type 1,” they wrote.
SMA type 1 typically results in death or need for mechanical ventilation by age 2, often with feeding difficulties. In addition to mutations in the SMN1 gene, patients have a variable number of SMN2 genes, which may partially compensate for malign effects of nonfunctional SMN1.
STR1VE was an open-label, single-arm, single-dose, phase III trial. Treated patients (n=22) and a historical untreated comparison cohort (n=23) had biallelic SMN1 mutations and two copies of SMN2. Treatment was a one-time intravenous infusion of onasemnogene abeparvovec (1.1×1014 vector genomes/kg) with follow-up once weekly for a month, then monthly until age 18 months.
Primary efficacy endpoints were assessed with the Children’s Hospital of Philadelphia Infant Test of Neuromuscular Disorders (CHOP INTEND), a motor function scale (0–64 points, with higher scores indicating better motor function).
From October 2017 to November 2019, SMA type 1 patients (55% female) received onasemnogene abeparvovec at a mean age of 3.7 months. For treated infants compared with the untreated natural history cohort:
- 13 of 22 patients (59%, 97.5% CI 36%–100%) achieved independent sitting for 30 seconds or longer (vs 0 of 23 patients in the untreated cohort; P<0.0001) at 18 months; median age of achievement: 12.6 months.
- 20 of 22 patients (91%, 97.5% CI 79%–100%) survived without requirement of permanent ventilation at 14 months, compared with 6 of 23 patients in the untreated cohort (26%, 97.5% CI 8%–44%; P<0.0001).
- All 22 treated patients had at least one adverse event, most commonly fever and liver enzyme elevation.
- Most frequently reported serious adverse events were bronchiolitis, pneumonia, respiratory distress, and respiratory syncytial virus bronchiolitis, considered unrelated to treatment.
- Three serious adverse events were related or possibly related to treatment (two patients had elevated hepatic aminotransferases, and one had hydrocephalus requiring shunt placement).
“Although patients who received onasemnogene abeparvovec showed improvements in independent sitting for 30 seconds or longer and survival free from permanent ventilation that are unprecedented in untreated patients with spinal muscular atrophy, management of the disease with standards of care remains important after gene therapy,” Day and colleagues wrote.
“These results are unequivocally positive in the context of a well described progressive and lethal disease, nevertheless the STR1VE study has shortcomings that are inherent to interventional studies in rare life-threatening diseases: the small sample size due to the limited number of patients available, and the open-label aspect of the study for ethical reasons,” observed Nathalie Goemans, MD, PhD, of University Hospitals Leuven in Belgium in an accompanying editorial.
“The authors have compared their results with the best available natural history data, but differences in baseline characteristics of ventilation and nutritional support between the cohorts suggest that patients in the historical cohort had more severe disease, which might result in possible overestimation of the results.”
Natural history studies have shown that the median age at death or permanent ventilation for SMA type 1 with two copies of SMN2 is 10.5 months and 8 months, respectively. Two other FDA-approved treatment options for SMA exist besides onasemnogene abeparvovec. Nusinersen (Spinraza) is an antisense oligonucleotide given as lifelong intrathecal dosing that was approved in December 2016; risdiplam (Evrysdi) is an SMN2 splice modifier given in a daily oral dose, approved by the FDA in August 2020. Onasemnogene abeparvovec is given as a one-time intravenous infusion and was approved in May 2019.
Day and colleagues compared treated patients in the present study with a historical cohort of untreated infants from the Pediatric Neuromuscular Clinical Research Network study. From a mean baseline CHOP INTEND score of 32, early and sustained improvement was seen in treated patients: increases of 6.9 points at 1-month post-dosing, 11.7 at 3 months, and 14.6 points at 6 months. A CHOP INTEND score of 40 or better was seen in 21 (95%) patients, while 14 (64%) achieved 50 points or more, and 5 (23%) 60 or better at any time during the study.
“Children with spinal muscular atrophy type 1 almost never achieve or maintain CHOP INTEND scores greater than 40 points,” the researchers pointed out.
Ability to thrive, a composite secondary endpoint that required the ability to tolerate thin liquids, feeding only by mouth, and maintaining weight greater than the third percentile for age and sex, was met by nine (41%) treated patients versus vs 0 in the untreated cohort. Two deaths were reported, the researchers noted; both were considered unrelated to treatment.
Limitations include the study’s single-arm, open-label design. “Given the commercial licensing of an effective intrathecal antisense oligonucleotide therapy (nusinersen) for spinal muscular atrophy, a placebo-controlled study was unethical, but a single-arm study was justifiable,” the researchers said.
-
Onasemnogene abeparvovec, a gene therapy for spinal muscular atrophy (SMA), led to improvements in sitting and survival for infants with the most severe form of SMA, the phase III STR1VE trial found.
-
While patients who received onasemnogene abeparvovec showed improvements in independent sitting for 30 seconds or longer and in survival free from permanent ventilation that were unprecedented in untreated SMA patients, management of the disease with standards of care remains important after gene therapy, the researchers said.
Paul Smyth, MD, Contributing Writer, BreakingMED™
Novartis Gene Therapies funded this study.
Day reports research grant support from AMO Pharmaceuticals, Audentes, Biogen, Cytokinetics, Expansion Therapeutics, Ionis Pharmaceuticals, Novartis Gene Therapies, Pfizer, Roche, Sanofi-Genzyme, Sarepta Therapeutics, Scholar Rock, SMA Foundation, CureSMA, and the Muscular Dystrophy Association. He has also received support for consulting or advisory board activities with Affinia Therapeutics, Avidity Therapeutics, Biogen, Cytokinetics, Kate Therapeutics, Novartis Gene Therapies, Pfizer, Roche, Sarepta Therapeutics, Scholar Rock, and the Muscular Dystrophy Association.
Goemans declared personal fees from Biogen, Roche, and Avexis outside the submitted work.
Cat ID: 130
Topic ID: 82,130,730,130,138,192,925