1. Patients who underwent catheter drainage for infected necrotizing pancreatitis did not experience better post-interventional outcomes compared to postponed drainage.
2. Patients who underwent postponed drainage required fewer invasive interventions.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Infected necrotizing pancreatitis often requires interventional treatment of catheter drainage and antibiotic administration. However, the therapeutic benefit of the timing of this drainage to be performed at diagnosis, compared to after the infection has encapsulated, is unclear. In this randomized controlled trial, 104 patients with infected necrotizing pancreatitis were randomized to either receive immediate or postponed catheter drainage. The therapeutic efficacy of the intervention was primarily measured using the Comprehensive Complication Index (CCI) The study found no differences in mean CCI scores or mortality between the two groups. Moreover, the cohort receiving postponed drainage experienced fewer interventional treatments (subsequent catheter drainage or necrosectomy) compared to the immediate drainage group. The results of this study were primarily limited by the measure of complications, as the CCI is primarily used to measure postoperative complications where some factors may not be clinically relevant. The study also did not differentiate between endoscopic from surgical drainage events, which may influence the efficacy of the intervention. Together, this study found no benefit in therapeutic outcomes in infected necrotizing pancreatitis patients receiving immediate catheter drainage compared to those treated with a more conservative postponed drainage approach.
Click to read the study in NEJM
Relevant Reading: Timing of surgical intervention in necrotizing pancreatitis
In-Depth [randomized controlled trial]: In this multi-center, randomized controlled trial, 932 patients with necrotizing pancreatitis were assessed. Patients were enrolled in the trial if they had an infection confirmed by imaging, or by Gram’s stain or culture from a biopsy sample. Patients were randomized in a 1:1 ratio to either receive immediate catheter drainage and antibiotics upon diagnosis or postponed intervention until encapsulated necrosis was observed. Additional interventions including catheter tube replacement or necrosectomy were considered if clinical improvement was not observed within 72 hours of intervention. For the primary outcome, patients were followed for 6 months for improvements in clinical complications, which was measured as a Comprehensive Complication Index (CCI) score. Secondary outcomes included mortality rate, number of interventions, and incidence of major complications. The study found no differences in mean CCI score between the immediate (CCI score, 57; 95% confidence interval [CI], 50-65) and the postponed drainage group (CCI score, 58; 95% CI, 50-67). No differences were found in mortality rate (relative risk [RR], 1.25; 95% CI, 0.42-3.68) or major complications (RR, 0.94; 95% CI, 0.77-1.14). However, for interventions, the immediate drainage group had a higher average number of interventions (4.4 vs. 2.6), increased risk for necrosectomy (RR, 2.27; 95% CI 1.27-4.06 ). In fact, 19 (39%) patients treated conservatively did not receive catheter drainage because they improved from antibiotic therapy alone. Overall, this study demonstrates that while immediate drainage did not negatively impact outcomes but may increase the necessity of more therapeutic interventions compared to postponed drainage. Accordingly, a conservative approach first utilizing a course of antibiotics is supported.
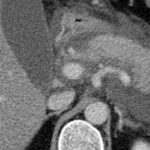
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.