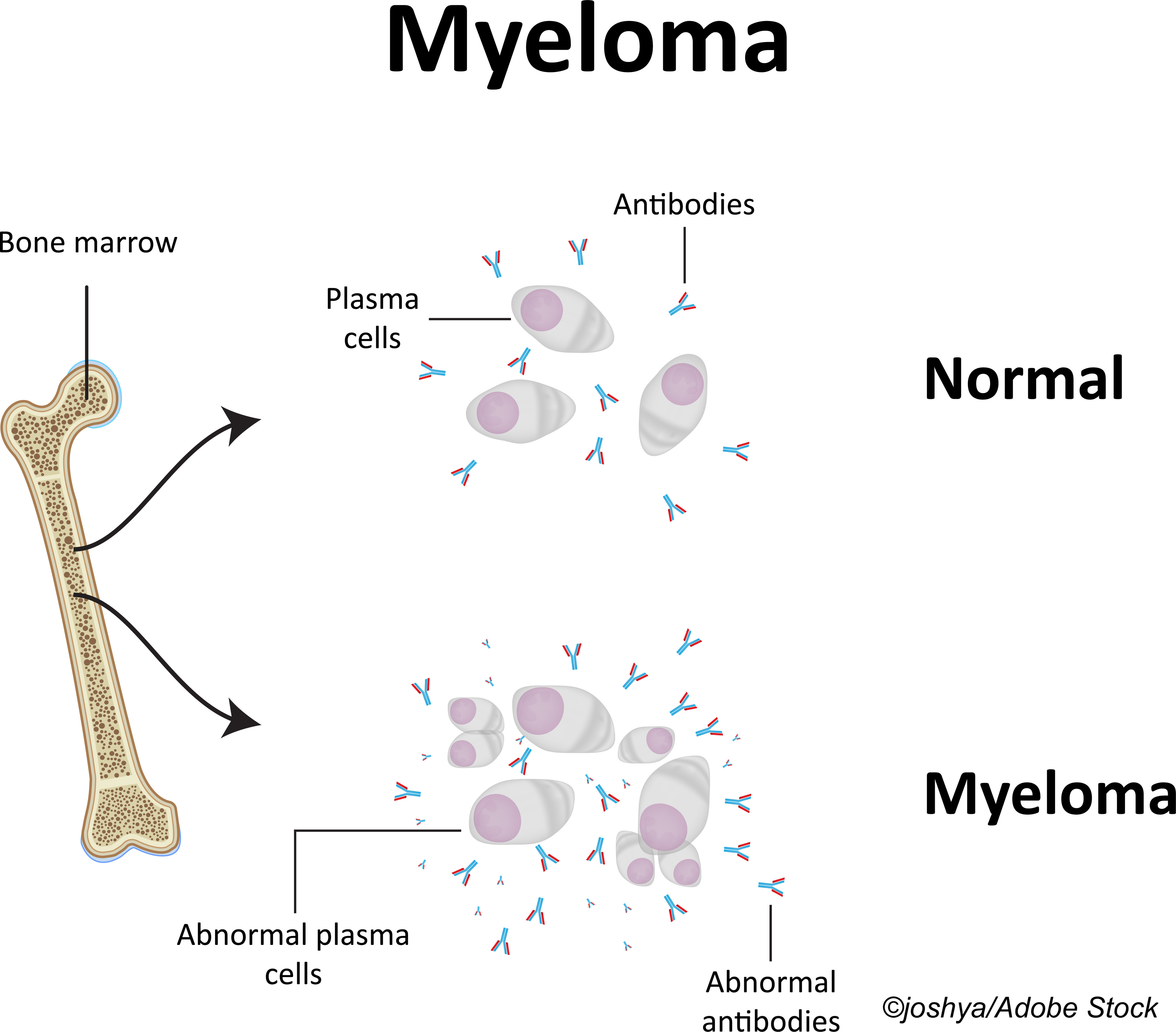
ATLANTA—The depth of response to first-line therapy for patients newly diagnosed with multiple myeloma is crucial, as it is predictive of long-term outcome, yet many patients—especially elderly patients—will need to proceed to second-line therapy.
Slavisa Ninkovic, MBBS, of the University of Melbourne and St. Vincent’s Hospital Melbourne, and colleagues said published data suggest that as many as two-thirds of multiple myeloma patients who are ineligible for transplant will require second-line therapy, and currently the standard-of-care for second-line treatment for elderly or frail patients is lenalidomide in combination with dexamethasone.
“But one in five patients do not achieve a partial response after four months of therapy,” Ninkovic explained in a poster presentation at the American Society of Hematology 2021 meeting. “What is concerning is that, continued on that regimen for another six months, just over a third (37%) of these patients will actually be converted to a partial response. While we need to do better in this cohort of patients, this should not come at the expense of increased treatment-related toxicity or financial burden.”
In a phone interview with BreakingMED, S. Vincent Rajkumar, MD, a professor of medicine at the Mayo Clinic in Rochester, explained that the concept described by Ninkovic is a good one—to add-on an agent when a patient fails to achieve at least partial response—but in the U.S., “we never start with a doublet but rather always start with a triplet.”
That said, he pointed out that in the U.S., there are currently several studies testing efficacy of so-called quad or four-drug regimens.
The phase II IRIL study of the Australian Myeloma Research Consortium (AMaRC 18-02) was a “multicenter, response-adapted study examining treatment intensification with isatuximab, an anti-CD38 monoclonal antibody,” for patients who failed to achieve response on lenalidomide/dexamethasone alone.
The trial enrolled treatment-naive, non-transplant eligible multiple myeloma patients. The patients were initiated on lenalidomide at 25 mg on days 1-21 of a 28-day cycle and dexamethasone at 40 mg (a 20 mg dose was used for patients age 75 or older). Patients who failed to achieve a partial response after four cycles (four months) or did not achieve a very good partial response after six cycles or who had progressive disease were eligible for add-on therapy with isatuximab (10 mg/kg weekly for one cycle and then every two weeks). Isatuximab was discontinued in patients who had progressive disease or adverse events. Patients who achieved the targeted response on lenalidomide/dexamethasone were maintained on that index therapy.
The primary endpoint was the rate of partial response following six cycles of the isatuximab/lenalidomide/dexamethasone combination treatment in patients who failed to achieve partial response on index treatment. As secondary endpoint, the researchers evaluated “the depth of response, progressive-free response, and overall response and safety.”
“At the time of data cut-off, we had recruited 42 patients, median age 77.7 years,” Ninkovic said. Just over half (n=22) were men.
The R-ISS breakdown was as follows:
- Stage I=19.7% (n=8).
- Stage II=54.8% (n= 23).
- Stage III=16.7% (n=7).
Ninkovic said R-ISS status was not available for four patients (9.5%).
“In total, 25 patients have had treatment intensification with isatuximab,” he said. Eighteen of the 25 have had at least six months of intensified therapy with isatuximab with increased depth of response observed in two-thirds (n=12). “Nine patients rescued with isatuximab after not reaching a target response with lenalidomide/dexamethasone have completed six cycles of the intensified therapy with all achieving a deepening of response—five patients achieved partial response and four achieved very good partial response,” Ninkovic said.
The median follow-up time was just short of 10 months.
The most common adverse events were infections, neutropenia, insomnia, and mood disorders. One patient on lenalidomide/dexamethasone reported grade 4 neutropenia. “There were fewer grade 3 or grade 4 events reported among patients on the isatuximab combination than on the standard rescue regimen, and causality was less frequently attributed to isatuximab.”
Ninkovic concluded that “for the elderly or frail newly diagnosed [with] transplant ineligible myeloma, isatuximab intensification upon inadequate response to standard-of-care lenalidomide-dexamethasone is both safe and effective.” He noted that this approach to intensification “leads to universal deepening of response in patients who failed initial rescue therapy without increasing toxicity.”
-
Findings from a small, multicenter study by Australian researchers suggest that intensification of standard second-line lenalidomide/dexamethasone therapy with the addition of isatuximab can boost partial response rates among elderly multiple myeloma patients.
-
Be aware that these findings were reported in a medical conference and should be regarded with caution until published in a peer-reviewed journal.
Peggy Peck, Editor-in-Chief, BreakingMED™
The study was supported by Sanofi/Genzyme.
Ninkovic had no disclosures.
Cat ID: 118
Topic ID: 78,118,730,118,121,332,468,935,192,925,331