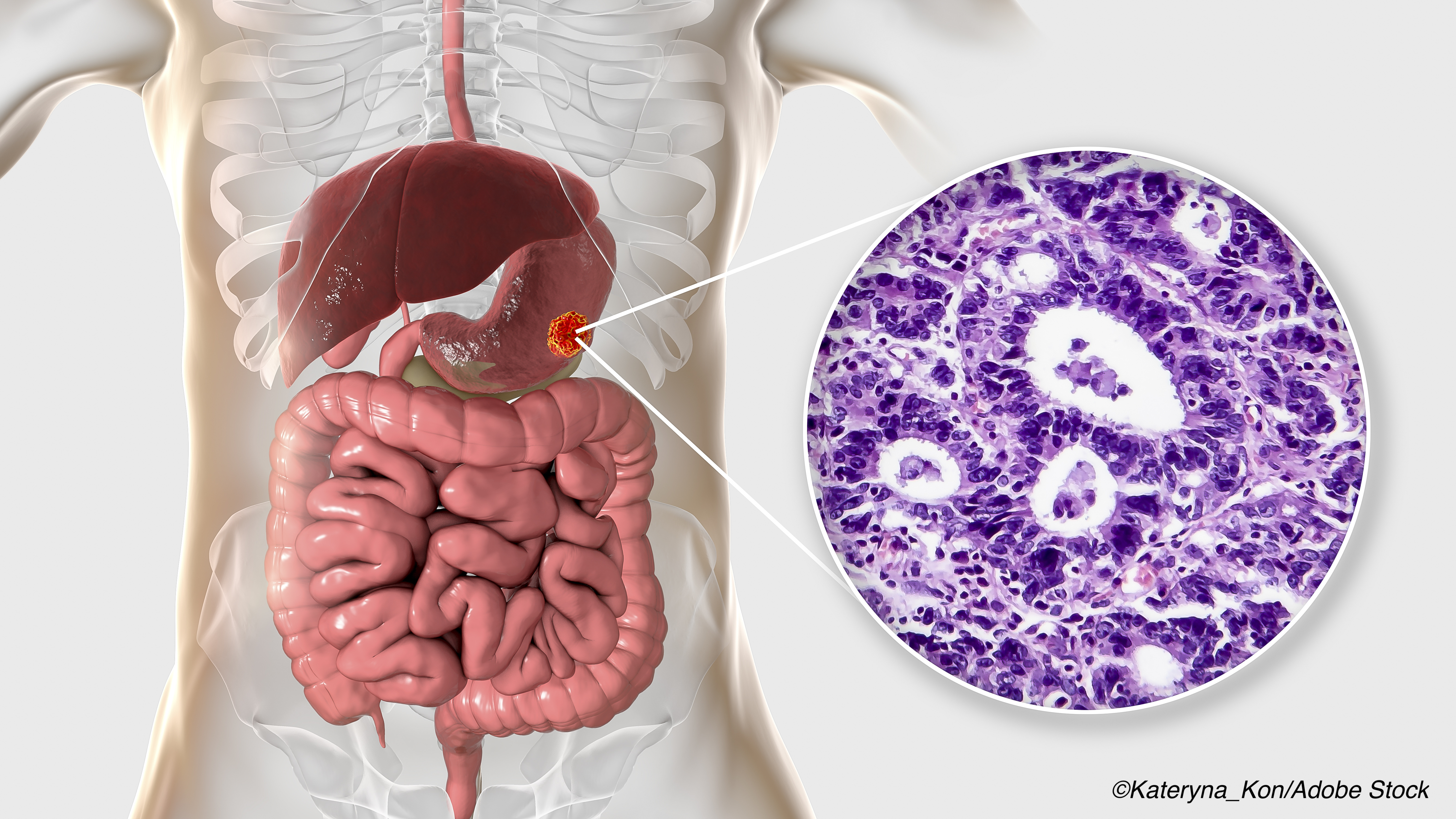
Middle segmental gastrectomy (MSG)—with dissection of stations 1, 3, 4sb, 4d, 7, 8, 9, 11p, and 12a—is feasible and recommended for middle- and high-body gastric cancers, according to a study published in JAMA Network Open.
Results supported the importance of metastatic lymph nodes in the management of gastric cancer, with researchers finding low rates of lymph node metastasis to key stations for CT1NO/1MO tumors (stations 5 and 6) and well-differentiated cT2NO/1MO tumors <4 cm in the middle- or high-body of the stomach.
“For the treatment of middle-body (MB) and high-body (HB) [gastric cancer] GC, distal gastrectomy and total gastrectomy are recognized as standard, safe procedures. However, these procedures are associated with post-gastrectomy syndromes that reduce the patient’s quality of life. Function-preserving procedures, such as pylorus-preserving gastrectomy (PPG), segmental gastrectomy (SG), and proximal gastrectomy (PG), with more limited lymph node (LN) dissection, can improve postoperative quality of life in selected patients,” wrote Harbi Khalayleh, MD, and colleagues.
From among over 9,000 patients who underwent surgical management of gastric cancer, Khalayleh and fellow researchers included 701 patients (mean age: 56.35 years; 59.6% men) with gastric cancer in the middle- or high-body of the stomach who had undergone either laparoscopic, open total, or subtotal gastrectomy at the National Cancer Center in Goyang, Korea
Patients were followed-up for at least three years, and the primary outcome of the study was the rate of metastasis at lymph node stations that cannot be dissected during MSG (2, 4sa, 5, 6, and 11d). Researchers defined MSG as “a small-circumferential gastric resection preserving the cardia and pylorus, excluding PPG.”
Upon analysis, Khalayleh and fellow researchers found that the incidence of lymph node metastasis was 0% in the following, regardless of size and differentiation:
- Station 5 for cT1-3NO/1MO cancers.
- Station 4sa for CT1-2NO/1MO cancers.
- Station 2 for CT1NO/1MO cancers.
- Station 6 for CT1N1MO cancers.
- Station 11d for CtIN1MO-ct2NO/1MO cancers.
- Station 12a for CT1NOMO cancers.
The rates of lymph node metastasis for CT1NOMO cancers were 0.3% at station 6 and 0.8% at station 11d.
Tumor metastasis occurred significantly more often in tumors that were ≥4.1 cm (OR: 2.10; 95% CI: 1.20-3.67; P=0.009), and the overall incidence of lymph node metastasis was also high compared with those ≤4 cm (32.8% versus 18.8%).
Rates of metastasis at key stations were lower in tumors ˂4 cm compared with those 4.1 cm or larger. For example, at station 2, rates of metastasis were 2.4% versus 9.8%, respectively; at station 4sa, 1.3% versus 2.5%; at station 5, 0% versus 0%; at station 6, 0.4% versus 3.7%; and at station 11d, 1.4% versus 4.3%.
In addition, lymph node metastasis in tumors ≤2 cm was also low (1.9% at station 2, 1.4% at station 4sa, 0% at station 5, 0.3% at station 6, and 0% at station 11d, and 0.5% at station 12a.
Finally, compared with poorly differentiated tumors, tumors that were well-differentiated were associated with a lower risk of lymph node metastasis (OR: 2.88; 95% CI: 1.45-5.73; P=0.002).
In an accompanying editorial, Helen Pham, MBBS, MS, MPH, of Westmead Hospital, Westmead, New South Wales, Australia, and Arthur J. Richardson, MBS, DClinSurg, of The University of Sydney, Sydney, New South Wales, Australia, lauded these results from Khalayleh and colleagues.
“MSG is not a procedure commonly performed in western countries but is more popular in eastern countries where there is a higher rate of [gastric cancer] GC and where there may be an increased percentage of early GC diagnosed. One of the obstacles to the broader application of MSG has been the concern about regional metastatic disease, and the study by Khalayleh and colleagues has provided valuable insight into the metastatic load in the various lymph node stations. In early reports, it does appear that MSG is accompanied by decreased morbidity and specifically a reduction in early dumping syndrome and reflux gastritis symptoms,” they wrote.
They added that these results may help clinicians and surgeons in the decision-making process for other minimally invasive treatments for gastric cancers, such as endoscopic mucosal resection for patients with early gastric cancers.
“It is certain that the treatment of GC will change substantially in the decades to come and will, hopefully, be less morbid and more effective for our patients. This study by Khalayleh et al is a valuable addition to our current knowledge of the patterns and rate of LN metastasis in GC and has provided a useful signpost in the selection of patients for minimally invasive gastrectomy and may help us to develop more robust indications for EMR,” they concluded.
Study limitations include its retrospective nature, the possibility of some stage migration between T2 and T3 tumors, and the lack of detailed lymph node data in some patients.
-
Middle segmental gastrectomy with dissection of LN stations 1, 3, 4sb, 4d, 7, 8a, 9, 11p, and 12a can be recommended for high-body and middle-body cT1N0/1M0 gastric cancers 4 cm or smaller and well-differentiated cT2N0/1M0 cancers.
-
Dissection of LN stations 5 and 6 may not be needed in patients with gastric cancer with middle- and high-body tumors of ≤4 cm.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
This study was supported by the National Cancer Center, Korea.
Khalayleh, Pham, and Richardson reported no conflicts of interest.
Cat ID: 120
Topic ID: 78,120,730,120,935,192,925