Hospitals that adopted transcarotid artery revascularization (TCAR) as an option for carotid revascularization saw a 10% reduction in perioperative major adverse cardiovascular events (MACE) in patients with carotid artery stenosis, according to a registry-based study, although other quality-of-care initiatives may also have played a part.
In a study of data from the Society of Vascular Surgery’s Vascular Quality Initiative (VQI), the crude rate of MACE was similar for post-TCAR and post-CEA at 2.3% versus 2.4% (P=0.91), reported Jesse A. Columbo MD, MS, of the Dartmouth-Hitchcock Medical Center in Lebanon, New Hampshire, and co-authors.
The rate of MACE over time decreased for CEA from 2.5% in 2015 to 1.9% in 2019 (P<0.001 for trend), as did the rate of MACE for TCAR, at 3.1% in 2016 versus 2.2% in 2019, but the change was not statistically significant (P=0.07 for trend), they explained in JAMA Network Open.
“This comparative-effectiveness study found that among more than 85,000 patients treated across 469 centers, TCAR adoption was associated with a 10% lower likelihood of perioperative MACE after TCAR and CEA combined versus if the center had continued to perform CEA alone,” the authors wrote. “These findings suggest that the adoption of TCAR as an option for carotid revascularization, making it available for select patients for whom it is the best treatment option, is associated with better overall performance.”
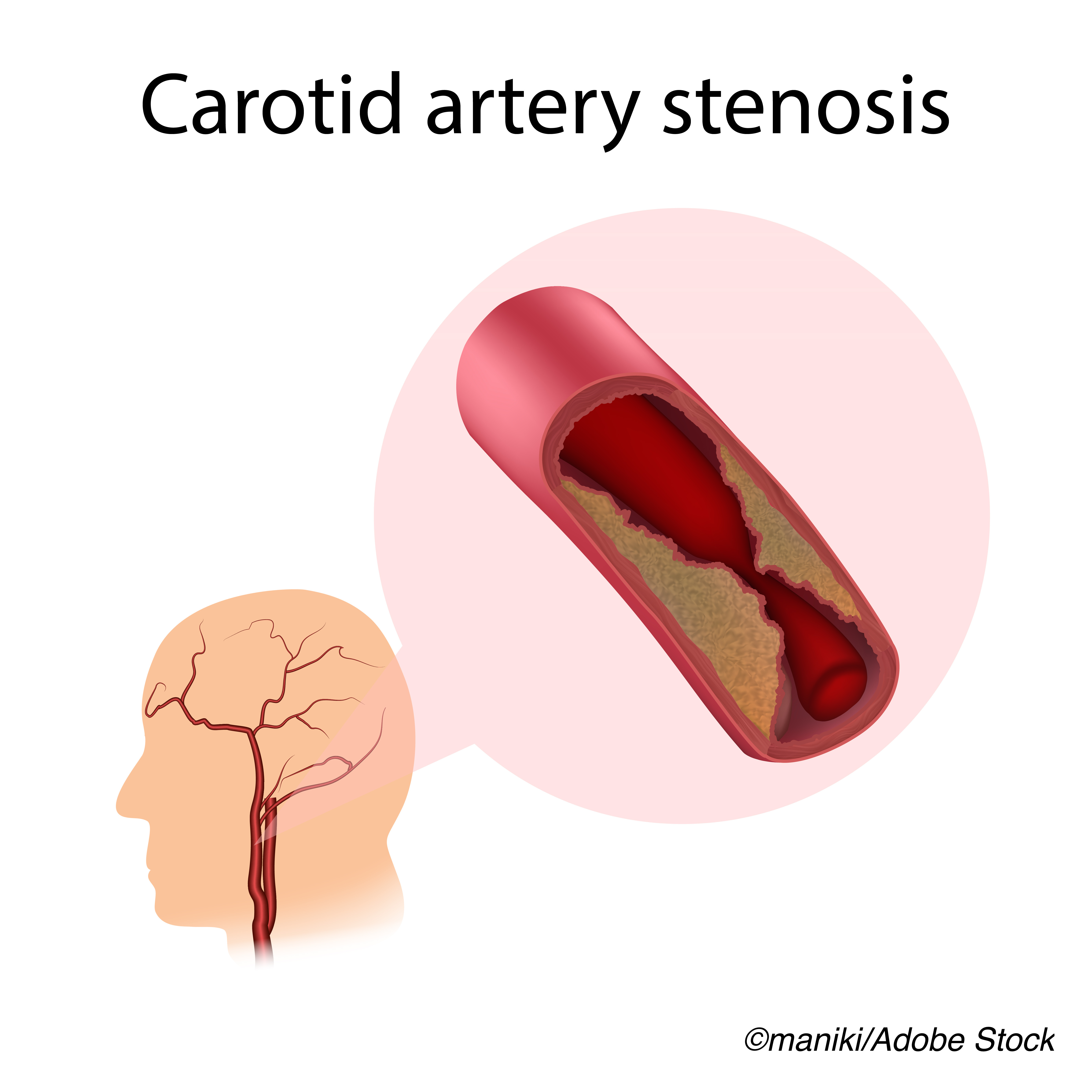
In an invited commentary accompanying the study, Peter W. Groeneveld, MD, MS, of the University of Pennsylvania Perelman School of Medicine in Philadelphia, noted that carotid arterial revascularization is a high-risk procedure, with 4%-5% of patients experiencing MACE. But it is still the evidence-based cornerstone for symptomatic or severe asymptomatic carotid atherosclerosis, he added.
Yet “The primary threat to this study’s validity is whether TCAR adoption by a hospital was associated with other concurrent quality-of-care initiatives that were the actual effectors of lower MACE rate,” he stated. “For example, it would not be surprising if TCAR-adopting hospitals were on a different trajectory for surgical quality than hospitals that did not adopt TCAR or did so slowly.”
“What’s needed is a randomized clinical trial of patients who are eligible for either procedure in order to “dispel any lingering doubts regarding TCAR’s comparative effectiveness,” Groeneveld added.
Still, he acknowledged that “the preponderance of existing observational data and evidence from single-group trials certainly supports TCAR’s noninferiority to CEA, and in combination with a 2020 comparative effectiveness observational study using standard multivariable regression, the findings by Columbo et al are approaching the limit for nonclinical trial data to inform questions regarding TCAR’s safety and effectiveness.”
TCAR was FDA approved in 2015 and is performed via a low neck incision with a direct carotid arterial puncture, using flow-reversal embolic protection before manipulation of the carotid atherosclerotic lesion, the authors explained.
“These features of TCAR remove the need to traverse the aortic arch and carotid lesion prior to embolic protection that is necessary with transfemoral carotid stenting, and early results with TCAR have been favorable,” they said, adding that it has become a valuable option in patients with challenging anatomy, such as a high carotid artery bifurcation or a carotid lesion close to the skull base, both of which make traditional CEA technically difficult.
The authors conducted a difference-in-difference analysis of retrospective (2015-2019) data from the VQI to determine the center-level association of TCAR adoption with overall perioperative outcomes for TCAR and CEA combined at more than 400 North American centers performing both procedures.
After FDA approval, the number of centers performing both TCAR and CEA increased from 15 centers in 2015 to 247 centers in 2019, for a >16-fold increase. In addition, the proportion of all carotid procedures that were TCARs increased from 0.7% in 2015 to 17% in 2019, for a 24-fold increase, they reported.
The study’s main outcome and measure of the study was the rate of MACE at these facilities. More than 86,000 patients underwent revascularization for carotid artery stenosis, 8.9% of whom got TCAR (mean age 73.1; 36.4% women; 90.6% White; 48.8% symptomatic) while 91.1% underwent CEA (mean age 70.6; 39.5% women; 90.2% White; 48.3%) symptomatic).
The difference-in-difference analysis demonstrated the benefit of adding TCAR to the carotid arterial revascularization menu, with a 10% decrease in the likelihood of MACE at 12 months after TCAR adoption versus if those centers had continued to perform CEA alone (odds ratio 0.90, 95% CI 0.81 to 0.99, P=0.04), Columbo’s group said.
Study limitations included the fact that VQI captures a smaller proportion of CEA procedures in North America, which may limit generalizability of study results to facilities that do not participate in the VQI. Also, data in the VQI is self-reported and may be associated with reporting bias.
Groeneveld stressed that “the findings do not imply that all carotid procedural recipients at TCAR-adopting hospitals had comparable or better outcomes than all carotid procedural recipients at CEA-only hospitals. For example, it is possible that the benefits derived from improved sorting of patients to TCAR or CEA may have masked potential harms from inappropriate recruitment of high-risk cases that ought to have been managed nonsurgically.”
-
Centers that adopted transcarotid artery revascularization (TCAR) in addition to post-carotid endarterectomy (CEA) had a lower likelihood of perioperative cardiovascular events than if the centers had not adopted TCAR.
-
TCAR and CEA had similar perioperative results, but TCAR adoption may allow clinicians to personalize procedure selection for patients with carotid artery stenosis.
Shalmali Pal, Contributing Writer, BreakingMED™
Columbo reported no relationships relevant to the contents of this paper to disclose. Co-authors reported relationships with, and/or support from, the Research Advisory Committee for the Vascular Quality Initiative, the Transcarotid Artery Revascularization Steering Committee, the NIH, the Patient-Centered Outcomes Research Institute, Silk Road Medical, and the Safety and Efficacy Study for Reverse Flow Used During Carotid Artery Stenting Procedure (ROADSTER) 1 and ROADSTER 2.
Groeneveld reported no relationships relevant to the contents of this paper to disclose.
Cat ID: 914
Topic ID: 74,914,730,914,192,925,159



Create Post
Twitter/X Preview
Logout