Edoxaban proved non-inferior to vitamin K antagonists (VKAs) in patients with atrial fibrillation (AFib) treated with transcatheter valves, according to the ENVISAGE-TAVI AF trial results, but there was an excess bleeding risk with the direct oral anticoagulant (DOAC).
In >1,400 patients who were followed-up for around 18 months, the primary efficacy outcome of composite net adverse clinical events (NACE) for edoxaban was 17.3/100 person-years (PY) versus 16.5/100 PY with VKAs, for a hazard ratio of 1.05 (95% CI 0.85 to 1.31, P=0.01 for noninferiority), according to George D. Dangas, MD, PhD, of Mount Sinai Medical Center, Icahn School of Medicine at Mount Sinai in New York City, and the rest of the ENVISAGE-TAVI AF investigators.
NACE consisted of all-cause death, myocardial infarction, ischemic stroke, systemic thromboembolism, valve thrombosis, and major bleeding.
Rates of major bleeding were 9.7/100 PY and 7.0/100 PY, respectively (HR 1.40, 95% CI 1.03 to 1.91, P=0.93 for noninferiority), and the difference between groups was mainly due to more gastrointestinal (GI) bleeding with edoxaban. Most patients experiencing major GI bleeds (82% and 96%), were also receiving concomitant treatment with proton-pump inhibitors, they explained in The New England Journal of Medicine. The results were simultaneously presented at the 2021 European Society of Cardiology (ESC) virtual meeting.
“The safety endpoint was higher in the edoxaban arm,” Dangas conceded to ESC TV. But in “further [investigation] of these findings, we found that the differences in bleed were attenuated when the edoxaban dose was adjusted down to 30 mg and also in patients without the prescription of concomitant oral antiplatelet therapy.” Dangas added that the group will follow up with a bleeding-related analysis of the results, but still stated that “I would say that this is a valuable new type of therapy with these patients after TAVI [transcatheter aortic valve implantation].”
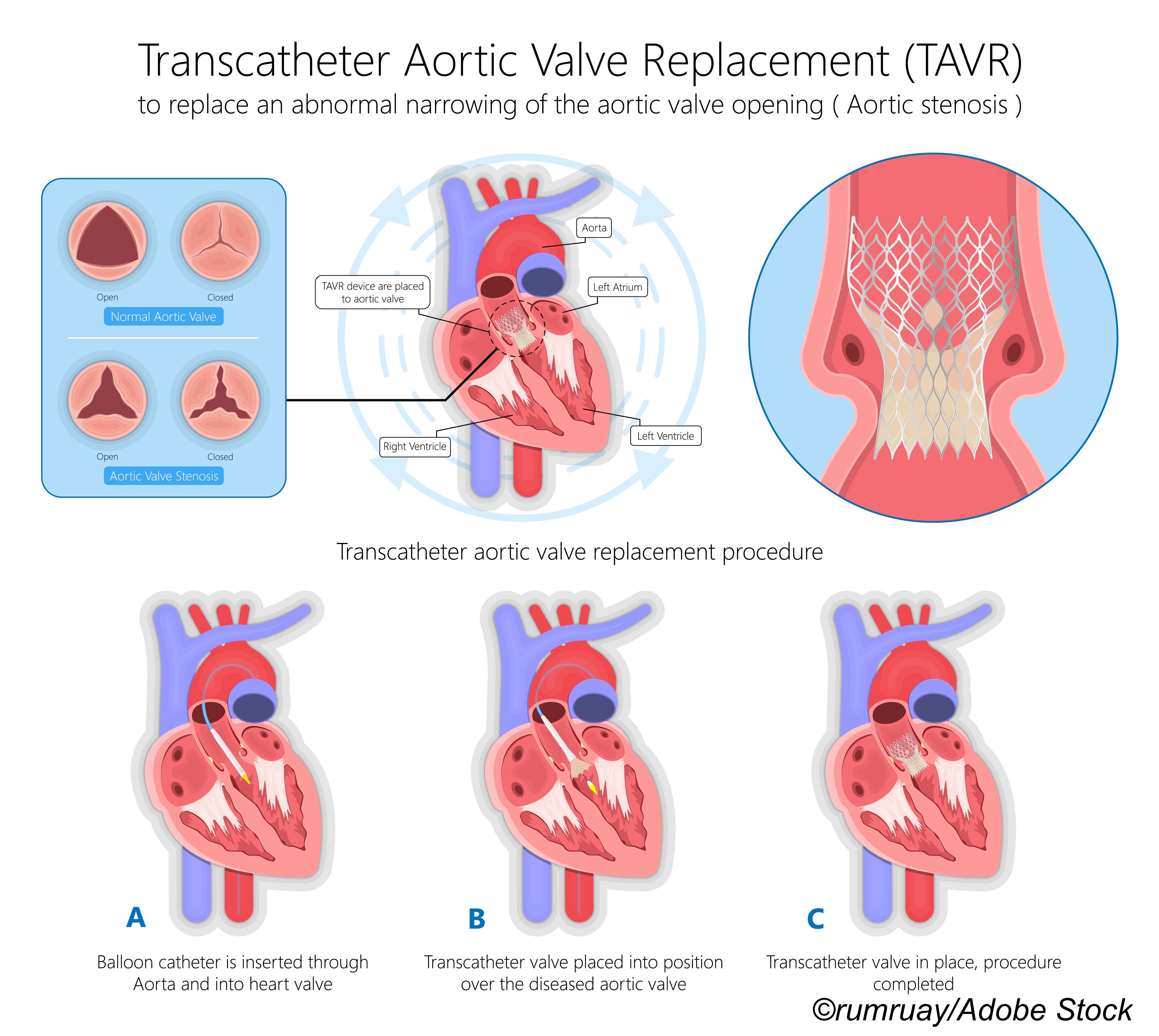
ENVISAGE-TAVI AF was done at 173 centers in 14 countries from April 2017 through January 2020. Patients had prevalent or incident AFib soon after receiving successful transcatheter aortic valve replacement (TAVR) for aortic stenosis.
Eligible patients (n=1,426; mean age 82.1; 47.5% women; about 83% White) were randomized in an open-label 1:1 fashion to either edoxaban (60 mg daily) or VKA with an international normalized ratio (INR) goal of 2-3. Specified antiplatelet therapy in either group was allowed at the discretion of the treating physician, including dual antiplatelet therapy for up to 3 months after TAVR or single antiplatelet therapy indefinitely.
Randomization largely occurred within 3 days after TAVR. The authors noted that 46.4% of patients in the edoxaban arm had a dose adjustment to 30 mg once a day on the basis of creatinine clearance, weight, or P-glycoprotein inhibitor use. Also, during the trial, 30.2% in the edoxaban group discontinued the trial agent versus 40.5% who quit a VKA.
The group overall had a mean Society of Thoracic Surgeons score of 4.9%, and a mean CHA2DS2-VASC score of 4.5. The vast majority (99%) had pre-TAVR AFib. Also, pre-randomization, there was concomitant use of oral antiplatelet agents in 46.0% of patients in the edoxaban group and 50.4% in the VKA group.
As for mortality, death from any cause or stroke occurred in 85 patients in the edoxaban group and in 93 patients in the vitamin K antagonist group (HR 0.86, 95% CI 0.64 to 1.15).
Trial limitations included the open-label design that increased the chance of reporting bias. Also, the pandemic in 2019 may have “affected the outpatient clinic follow-up routine and may have resulted in underassessment of laboratory data and mild-to-moderate clinical events,” the authors explained.
What might the results mean for the future of DOACS/NOACS (novel oral anticoagulants)? In an American College of Cardiology (ACC) summary, Dharam J. Kumbhani, MD, SM, of the UT Southwestern Medical Center in Dallas, pointed out that the “[ENVISAGE-TAVI AF] results are overall similar to data with edoxaban among patients with AFib but not undergoing TAVR; the higher bleeding rates are likely a reflection of the population enrolled: elderly and frail with multiple comorbidities,” and cited previous trials such as GALILEO (also led by Dangas) and ATLANTIS.
“I think the [non-inferiority results] were good in general for NOACS,” noted Deepak Bhatt, MD, MPH, of Brigham & Women’s Hospital in Boston, in an ESC Highlights discussion from the ACC. But Bhatt, who said he served on the ENVISAGE-TAV AF data and safety monitoring board, added that “In the U.S., I don’t know many folks… that are using edoxaban as their NOAC of choice. I think most folks will continue to use other NOACs.”
In the new valvular disease guidelines from ESC/European Association for Cardio-Thoracic Surgery, also presented at the ESC virtual meeting and published in the European Heart Journal, DOACS were strongly recommended over vitamin K antagonists in multiple indications, including stroke prevention in people with native valve disease and atrial fibrillation.
-
Edoxaban was non-inferior to vitamin K antagonists (VKA) for the composite primary outcome of adverse clinical events in patients who had an indication for oral anticoagulation for atrial fibrillation after successful transcatheter aortic valve replacement.
-
Edoxaban was tied to a higher risk of major bleeding than versus VKA in the ENVISAGE-TAVI AF trial.
Shalmali Pal, Contributing Writer, BreakingMED™
ENVISAGE-TAVI AF was funded by Daiichi Sankyo. Some co-authors are company employees.
Dangas reported relationships with, and/or support from, Bayer, Boston Scientific, Daiichi Sankyo, and Medtronic. Co-authors reported multiple relationships with industry including Daiichi Sankyo.
Cat ID: 913
Topic ID: 74,913,730,913,192,925