Even post-acute coronary syndrome (ACS) patients with low baseline LDL cholesterol (LDL-C <70 mg/dL) benefited from the addition of ezetimibe (Zetia) to statin therapy, according to an evaluation of the IMPROVE-IT trial.
In the post-hoc analysis, “absolute differences in median LDL-C achieved at 4 months between treatment arms were similar (17 to 20 mg/dL), reported Robert P. Giugliano, of the TIMI Study Group in Boston, and co-authors.
The effect of ezetimibe/simvastatin versus placebo/simvastatin on the primary endpoint was consistent regardless of baseline LDL-C, they wrote in the Journal of the American College of Cardiology (P=0.95 for interaction):
- 50 to <70 mg/dL: hazard ratio 0.92 (95% CI 0.80 to 1.05).
- 70 to <100 mg/dL: HR 0.93 (95% CI 0.87 to 1.01).
- 100 to 125 mg/dL: HR 0.94 (95% CI 0.86 to 1.03).
The authors also found that, between treatment arms, normalized relative risk reductions per 1-mmol/L difference in achieved LDL-C at 4 months was as follows in patients with baseline LDL-Cs of (P=0.91 for interaction):
- 50 to <70 mg/dL: 21%.
- 70 to <100 mg/dL: 16%.
- 100-125 mg/dL: 13%.
And, no “significant treatment interactions by baseline LDL-C were present for safety endpoints,” Giugliano’s group noted.
The findings seem to address one of the limits of the original IMPROVE-IT results, as described in a 2014 American College of Cardiology expert analysis: “It is important… to remember that the trial was done in exclusively high-risk persons with a recent ACS so may not apply to lower risk persons; thus, the implications of this trial beyond the study population and the NNT [number needed to treat] values should be generalized with caution,” wrote Nathan D. Wong, PhD, of the University of California Irvine, and Michael Blaha, MD, MPH, of the Ciccarone Center for the Prevention of Heart Disease at Johns Hopkins in Baltimore.
In addition, a “factor reducing the applicability of IMPROVE-IT to practice is its use of a moderate-intensity statin, which deviates from the [2014] guideline recommendation to use high-intensity statins in all eligible patients with ACS…”[the] trial population was not closely reflective of current clinical practice, calling into question the applicability of ezetimibe/simvastatin use to current patients with ACS,” noted Thomas M. Maddox, MD, MSc, of the VA Eastern Colorado Health Care System in Denver, and co-authors in a 2017 JAMA Internal Medicine research letter.
In the current study, Giugliano’s group acknowledged that IMPROVE-IT’s use of 40-mg background simvastatin, with uptitration to 80 mg in selected patients, did not “represent a maximally potent statin regimen, as is recommended in current [2018] guidelines” and that the trial had “strict inclusion/exclusion criteria, including that the patients have high-risk ACS, and thus may not apply to all patients seen in clinical practice.” Still, they held firm that their results “extend current guideline recommendations.”
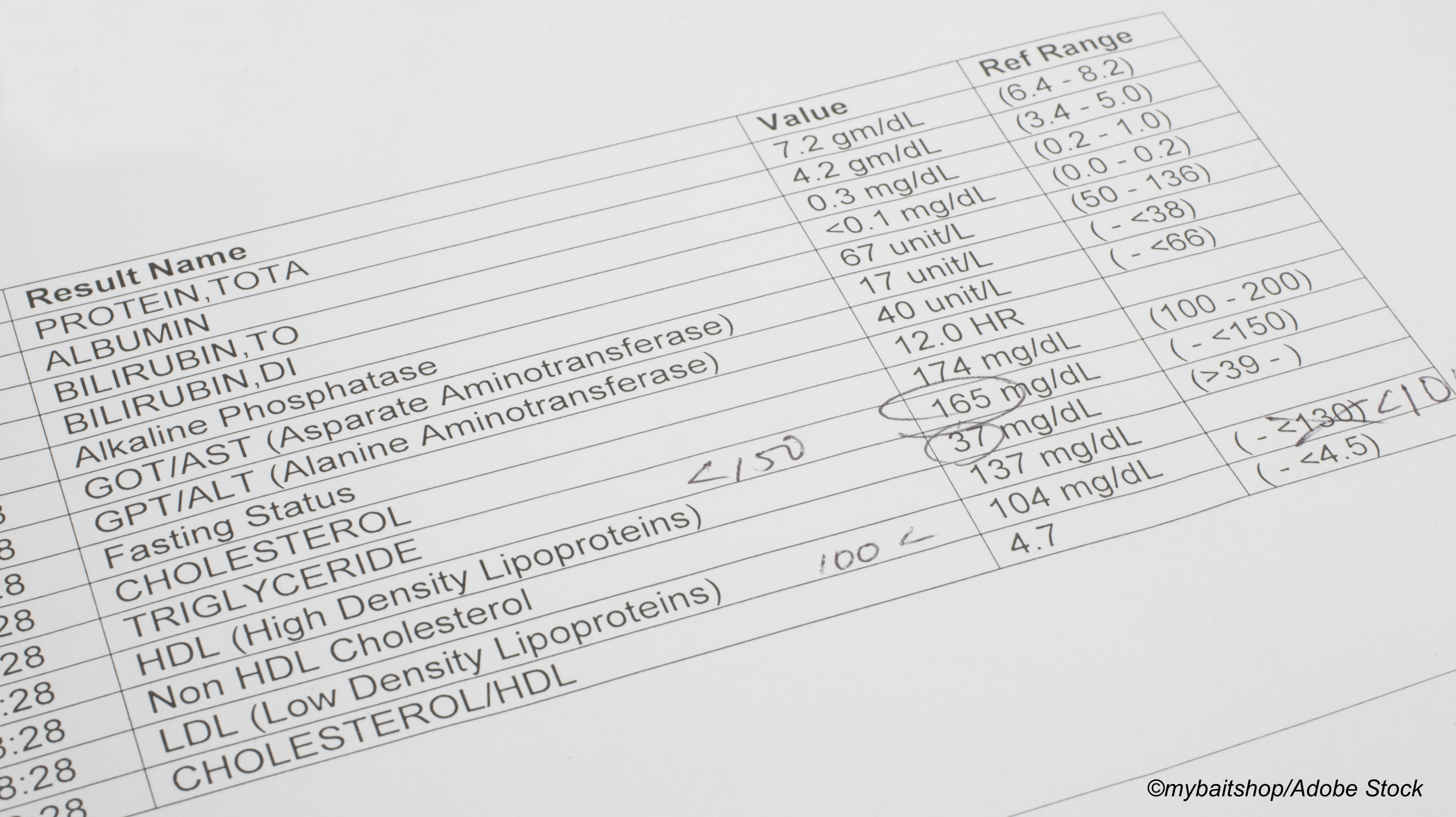
Giugliano and co-authors explained that IMPROVE-IT was a double-blind, placebo-controlled, randomized trial of ezetimibe/simvastatin versus placebo/simvastatin in post-ACS patients with a median of 6 years of follow-up. Nearly 18,000 patients were stratified by LDL-C at qualifying event into three groups: 50 to <70 mg/dL, 70 to <100 mg/dL, and 100 to 125 mg/dL. The trial’s primary endpoint was a composite of cardiovascular death, major coronary events, or stroke.
The goal of the current study was to “evaluate the relationship between baseline LDL-C level and the benefit of intensive lipid-lowering therapy (LLT) with the addition of ezetimibe to statin therapy in post ACS patients,” they explained.
In terms of adverse events (AEs), the authors noted that rates of AE-related discontinuation were similar with ezetimibe/simvastatin versus placebo/simvastatin across the various baseline LDL-C categories (treatment-subgroup P=0.60 for interaction):
- 50 to <70 mg/dL: 7.2% vs 7.8% (P=0.53).
- 70 to <100 mg/dL: 7.7% vs 7.2% (P=0.39).
- 100 to 125 mg/dL: 8.6% vs 8.0% (P=0.43).
Giugliano’s group highlighted study limitations—including the fact that the cut points of 70 and 100 mg/dL were post hoc—but emphasized that the “findings suggest that the magnitude of clinical benefit of ezetimibe/simvastatin in post-ACS patients is consistent and robust across the spectrum of baseline LDL-C from 50 to 125 mg/dL.”
In an editorial comment accompanying the study, Vera Bittner, MD, MSPH, of the University of Alabama at Birmingham, advised that “post-hoc subgroup analyses of randomized clinical trials should always be interpreted with some caution.”
She noted that participants in the lowest LDL-C group who had an ACS despite low LDL-C levels had many potentially confounding factors, such as older age, history of multiple chronic conditions, and being on pre-trial lipid-lowering therapy.
Ultimately, baseline “LDL-C viewed in isolation is not necessarily a reliable indicator of risk for recurrent events or of potential benefits of LDL-C lowering therapies and has to be interpreted in the context of the underlying ASCVD risk,” she stated. And “[g]iven the design of IMPROVE-IT, the current analysis cannot answer the question whether the LDL-C threshold for adding ezetimibe or PCSK9 inhibitor should be lowered to ≥50 mg/dL among individuals at very high ASCVD risk and using high-intensity statin therapy.”
She advised that the cardiology community “look beyond moderate-intensity statin therapy among our very-high-risk patients who cannot tolerate high-intensity statins, even if their baseline LDL-C levels are low.”
-
The addition of ezetimibe (Zetia) to simvastatin (Zocor) therapy safely and consistently reduced the risk of cardiovascular events in survivors of acute coronary syndrome across baseline LDL cholesterol (LDL-C) levels of 50 to 125 mg/dL.
-
Findings from the post-hoc analysis of the IMPROVE-IT trial extend current guideline recommendations in very-high-risk patients with low baseline LDL-C who cannot tolerate high-intensity statins.
Shalmali Pal, Contributing Writer, BreakingMED™
IMPROVE-IT was funded by the Merck. A co-author is a company employee.
Giugliano reported support from, and/or relationships with, Amgen and Anthos Therapeutics, Centrix, Daiichi-Sankyo, Dr Reddy’s Laboratories, Medical Education Resources, Medscape, Menarini, Pfizer, SAJA Pharmaceuticals, Servier, Voxmedia, Amarin, Bayer, CryoLife, Daiichi-Sankyo, Esperion, Gilead, Hengrui, Inari, PhaseBio Pharmaceuticals, St Lukes, and Sanofi.
Co-authors reported support from, and/or relationships with, JSPS Overseas Research Fellowships, Merck, Espirion, Sanofi/Duke Clinical Research Institute, Brigham and Women’s Hospital, Abbott, Amgen, Anthos Therapeutics, AstraZeneca, DaiichiSankyo, Eisai, Intarcia, MedImmune, Merck, Novartis, Pfizer, Regeneron Pharmaceuticals, Roche, The Medicines Company, Zora Biosciences, Merck Sharp and Dohme, Intarcia, IONIS, Quark Pharmaceuticals, Althera, Bristol Myers Squibb, CVS Caremark, DalCor, Dr Reddy’s Laboratories, Fibrogen, IFM Therapeutics, Moderna, Novo Nordis, Boehringer Ingelheim, Aegerion, Alnylam, Amarin, Applied Clinical Therapeutics, Ascendia, Corvidia, HLS Therapeutics, Innovent, Kowa, Eli Lilly, Rhoshan, Cardurion, MyoKardia, Ingelheim/Lilly, IMMEDIATE, and Verve.
Bittner disclosed relationships with the ODYSSEY OUTCOMES/Sanofi, STRENGTH/AstraZeneca, DalGene/Dalcor, CLEAR/Esperion, the University of Alabama School of Public Health/Amgen, ORION IV/Novartis, and Pfizer.
Cat ID: 4
Topic ID: 74,4,730,4,914,192,925



Create Post
Twitter/X Preview
Logout