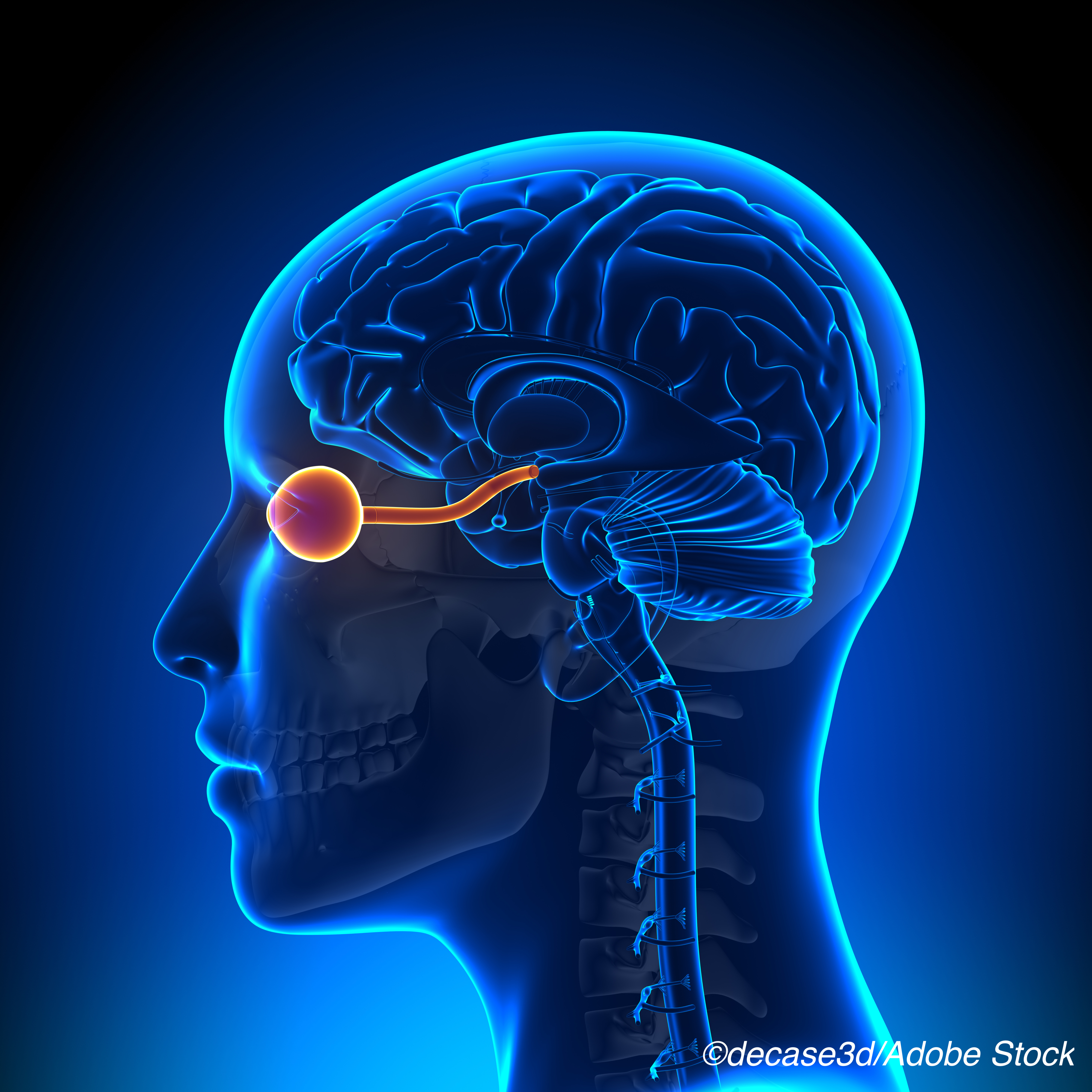
Including optic nerve lesions as part of diagnostic criteria improved sensitivity for diagnosing multiple sclerosis (MS) in a cohort with clinically isolated syndrome (CIS), an observational retrospective study showed.
“The addition of the optic nerve, assessed by visual evoked potentials (VEPs), as a fifth region in the current dissemination in space criteria slightly improves the diagnostic performance as it increases sensitivity without losing specificity,” wrote Angela Vidal-Jordana MD, PhD, of Universitat Autonoma de Barcelona in Spain, and co-authors in Neurology.
Four areas are included in current dissemination in space criteria: periventricular, cortico-juxtacortical, infratentorial, and spinal cord.
Vidal-Jordana and colleagues analyzed data from a 388-patient cohort with CIS — a first symptomatic attack suggestive of MS — to develop modified criteria including the optic nerve VEP results. Then they compared the diagnostic performance of the modified criteria with the 2017 McDonald criteria in a subset of participants (n=151) followed until a second attack suggesting MS, or for 10 years, whichever came first.
Compared with 2017 McDonald criteria, modified criteria showed:
- Increased accuracy: 78.1% versus 75.5%.
- Increased sensitivity: 82.3% versus 79.2%.
- No change in specificity: 52.4% for both.
Hazard ratios for a second attack were 4.3 (95% CI 2.8-6.5) for the 2017 McDonald Criteria and 4.8 (95% CI 3.0-7.5) for the modified criteria.
In an accompanying editorial, Wallace J Brownlee, MD, PhD, of University College London, and Steven Galetta, MD, of NYU Langone Health in New York City, wrote, “Improvement was mainly driven by the optic neuritis group, with more modest gains in patients with a non-optic neuritis presentation. These findings are consistent with a previous study where optic nerve involvement was assessed clinically (and in a subset of patients with VEPs) that found a benefit to including symptomatic but not asymptomatic optic nerve lesions in dissemination in space criteria.”
“The evidence base for including optic nerve lesions in MS diagnostic criteria is building,” they continued. “The study from Vidal-Jordana and colleagues confirms the value of VEP-detected optic nerve lesions, particularly in patients with acute optic neuritis. We now need prospective studies in CIS patients evaluating how more sensitive tools like orbital MRI and optical coherence tomography perform in this setting to help inform future revisions to the McDonald criteria.”
The 2017 revision of the 2010 McDonald criteria for the diagnosis of MS did not include the optic nerve as a diagnostic site due to lack of evidence that it added benefit but concluded that research to further refine the criteria should focus on optic nerve involvement, validation in diverse populations, and incorporation of advanced imaging, neurophysiological, and body fluid markers.
“This means that a symptomatic brain or spinal cord lesion can contribute to dissemination in space and time, but not a symptomatic optic nerve lesion, effectively setting the bar higher for a diagnosis of MS in patients with optic neuritis compared with other CIS presentations,” Brownlee and Galetta observed.
“Approximately 50% of patients with optic neuritis have asymptomatic brain and/or spinal cord lesions (indicating a high-risk for MS),” they added. “In fact, about one in five of these patients do not meet the McDonald 2017 criteria for dissemination in space, highlighting the frequency of this clinical quandary, and the potential for delays in the diagnosis and management of MS with our current diagnostic criteria.”
Vidal-Jordana and colleagues analyzed data from patients in the prospectively recruited Barcelona CIS cohort. All had MRI scans of the brain and spinal cord as well as VEPs near the time of presentation. Over 90% had abnormal MRI and almost 75% had cerebrospinal fluid-specific IgG oligoclonal bands. About 34% had a second attack within the 10 years following the qualifying CIS symptoms with mean time after CIS onset of 19.6 months.
Mean follow-up time was 62.7 months for the development cohort of 388 (mean age 33.5, 68% women, 54.3% positive oligoclonal bands) and about 89 months for the subset of 151 making up the diagnostic accuracy cohort (mean age 32.4, 72% women, positive 73.5% positive oligoclonal bands).
Abnormal VEPs were seen in 32.5% of the development cohort. Hazard ratios for a second attack tended to increase with increasing number of areas affected; for one through five affected areas, HRs were 5.6, 11.7, 15.8, 12.5, and 22.7, respectively.
“Our work provides additional evidence that argues in favor of including the optic nerve as a new region in the diagnostic criteria,” the researchers wrote. “Whether the optic nerve involvement in CIS patients should be confirmed only by means of VEPs, by the use of other structural tests (MRI or optical coherence tomography) or by a combination of them, requires further investigation in prospective studies with a systematic examination of the optic nerve in CIS patients.”
The use of VEPs to identify optic nerve lesions has both advantages and disadvantages, Brownlee and Galetta pointed out. “VEPs are widely available in most neurophysiology departments, with standardized international guidelines available for acquisition and interpretation, but testing is time-consuming requiring 30 minutes of physiologist and patient time,” they wrote.
-
Including optic nerve lesions as part of diagnostic criteria improved sensitivity for diagnosing multiple sclerosis (MS) in a cohort with clinically isolated syndrome, an observational retrospective study showed.
-
The 2017 McDonald criteria for MS diagnosis did not include the optic nerve as a diagnostic site due to lack of evidence that it added benefit, but concluded further research was needed.
Paul Smyth, MD, Contributing Writer, BreakingMED™
The study had no funding.
Vidal-Jordana receives support for contracts Juan Rodes from Fondo de Investigaciones Sanitarias, Instituto de Salud Carlos III, Spain and has engaged in consulting and/or participated as speaker in events organized by Novartis, Roche, Teva, Mylan, Biogen, Sanofi-Genzyme, and Merck.
Brownlee has received speaker honoraria for educational activities and/or participation in advisory boards for Biogen, Celgene, Merck, Mylan, Novartis, Roche and Sanofi Genzyme. Galetta has been a consultant for Biogen and Genentech.
Cat ID: 36
Topic ID: 82,36,730,36,192,925



Create Post
Twitter/X Preview
Logout