Treatment with a combination of the neprilysin inhibitor sacubitril and the angiotensin-receptor blocker (ARB) valsartan was not associated with a significantly lower incidence of death from cardiovascular causes or incident heart failure than ramipril, an angiotensin converting-enzyme (ACE) inhibitor, in patients with acute myocardial infarction (MI).
Over a median of 22 months, death from cardiovascular causes or incident heart failure occurred in 11.9% of the sacubitril-valsartan group and 13.2% of the ramipril group (HR 0.90, 95% CI 0.78-1.04, P=0.17) in the PARADISE-MI trial, reported Marc Pfeffer, MD, PhD, of Brigham and Women’s Hospital in Boston, and co-authors in The New England Journal of Medicine.
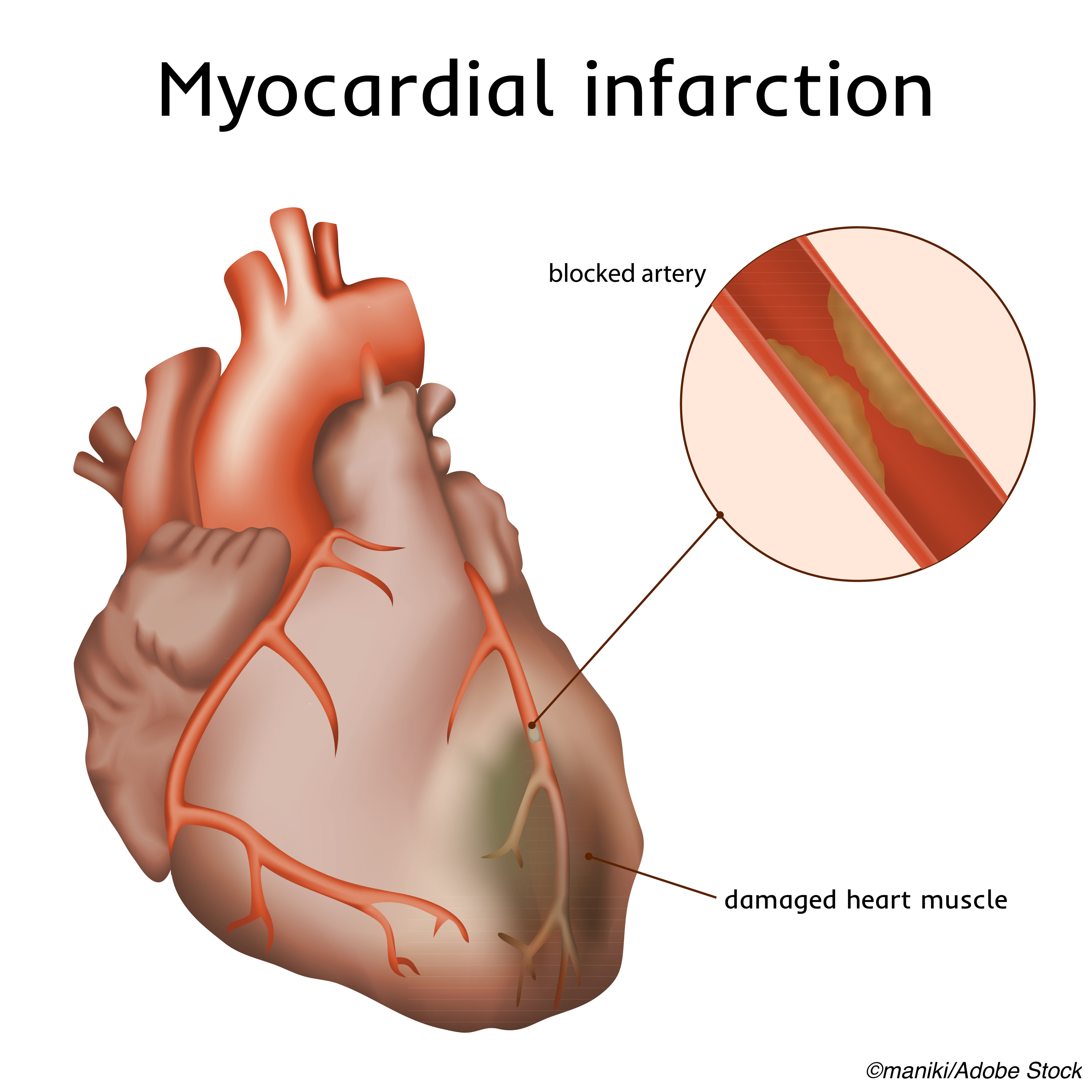
All participants had acute MI and either reduced left ventricular ejection fraction, pulmonary edema, or both, and no prior heart failure.
“Survivors of an acute myocardial infarction with a reduced left ventricular ejection fraction, transient pulmonary congestion, or both conditions were a relevant patient group because they remain at substantial risk for symptomatic chronic heart failure despite treatment advances, including prompt coronary reperfusion and treatment with statins,” Pfeffer and co-authors wrote.
“With the proven effectiveness of ACE inhibitors in this population, superiority to an active control therapy such as ramipril was required,” they continued. “Our objective, which was not met, was to show superiority of sacubitril-valsartan over ramipril in preventing the development of incident heart failure in this post-myocardial infarction population.”
The study “explored whether the benefits of angiotensin receptor-neprilysin inhibition over ACE inhibition would extend back from stable chronic heart failure into the context of acute myocardial infarction,” observed Lynne Stevenson, MD, and Andrew DeFilippis, MD, both of Vanderbilt University Medical Center in Nashville, in an accompanying editorial.
“The findings in PARADISE-MI do not support the use of an angiotensin receptor-neprilysin inhibitor before hospital discharge after an acute myocardial infarction, for which an ACE inhibitor or ARB is the guideline-recommended treatment,” they wrote. “For patients recovering a normal ejection fraction after myocardial infarction, ACE inhibitors and ARBs remain the recommended renin-angiotensin-aldosterone system inhibitors.”
“More neurohormonal inhibition is not always better,” Stevenson and DeFilippis added.
In PARADISE-MI, researchers randomized 5,661 patients with acute MI and either low ejection fraction, pulmonary edema, or both to sacubitril (target 97 mg)-valsartan (target 103 mg) twice daily (n=2,830) or ramipril with a target of 5 mg twice daily (n=2,831). Patients were followed for events from December 2016 through December 2020.
Randomization was a median 4.3 days after MI. All participants had one or more risk factors, including age 70 or older, diabetes, prior MI, estimated glomerular filtration rate <60 ml per minute per 1.73 m2 of body-surface area, atrial fibrillation, left ventricular ejection fraction of <30% associated with the index MI, Killip class III (acute pulmonary edema) or IV (cardiogenic shock or hypotension), or ST-segment elevation myocardial infarction without reperfusion within 24 hours after presentation.
Mean age of participants was 63.7 years and 24.1% were women. Coronary reperfusion had been attempted in 89.0% of the patients. The left ventricular ejection fraction was 40% or lower in 81.4% of participants, 54.0% had pulmonary congestion, and 35.5% had both at baseline. Overall, 78.4% were taking either an ACE inhibitor or ARB prior to the index MI before randomization; these medications were discontinued at randomization.
The composite primary outcome was death from a cardiovascular cause or incident heart failure (either hospitalization for heart failure or symptomatic outpatient heart failure), whichever came first.
For the primary outcome components, death from cardiovascular causes made up 40.5% of the sacubitril-valsartan outcome versus 36.5% of the ramipril outcome. Hospitalization for heart failure made up 48.5% versus 50.1%, and outpatient symptomatic heart failure made up 10.9% versus 13.4%, respectively.
Secondary outcomes that did not significantly differ between groups included death from cardiovascular cause or hospitalization for heart failure; death from combined cardiovascular cause, nonfatal MI, or nonfatal stroke; death from cardiovascular causes with total hospitalizations for heart failure, MI, or stroke; death from any cause; and heart failure requiring hospitalization or symptomatic outpatient heart failure.
Discontinuation of the trial drug for any reason other than death occurred in 17.7% of the sacubitril-valsartan group and 18.3% of the ramipril group. Discontinuation was due to adverse events in 12.6% and 13.4%, and hypotension occurred in 28.3% and 21.9%, respectively.
“Although the percentage of patients who discontinued their assigned medication was similar in the two groups, we did observe the expected pattern of more discontinuations attributed to hypotension and fewer attributed to cough with sacubitril-valsartan than with ramipril,” Pfeffer and colleagues noted.
“Several considerations are relevant when any major trial does not show a significant result with respect to the primary outcome, including the appropriateness of the trial population, the anticipated treatment effect, the primary outcome chosen, deficiencies in trial conduct, and the expected and actual statistical power,” the researchers pointed out.
“We believe that the conduct of our trial was satisfactory, with adequate adherence and minimal loss of data,” they added. “The trial also had sufficient power to detect the treatment effect size we had anticipated.”
-
Combination sacubitril and valsartan was not associated with a significantly lower incidence of death from cardiovascular causes or incident heart failure than ramipril in patients with acute myocardial infarction in the PARADISE-MI trial.
-
All participants in the PARADISE-MI trial had either reduced left ventricular ejection fraction, pulmonary edema, or both, and no prior heart failure.
Paul Smyth, MD, Contributing Writer, BreakingMED™
PARADISE was supported by Novartis.
Pfeffer disclosed consultant agreements with Astra Zeneca, Boehringer Ingelheim and Eli Lilly Alliance, Corvidia, DelCor, GlaxoSmithKline, Lexicon Pharmaceuticals, Inc., NHLBI CONNECTs, Novartis, Novo Nordisk, Pearbridge Health, and SANOFIT US SERVICES INC. Additionally, he disclosed stock options Pearbridge Health Inc. and DelCor as well as grant support from Novartis.
DeFillipis and Stevenson had nothing to disclose.
Cat ID: 3
Topic ID: 74,3,730,3,308,358,5,914,192,925