Parathyroidectomy was linked with “robust fracture risk reduction” in older adults with primary hyperparathroidism (PHPT), researchers reported.
In a population-based, longitudinal cohort study of all Medicare beneficiaries with PHPT, the unadjusted incidence of fracture was 10.2% in patients treated with parathyroidectomy at a mean follow-up period of 58.5 months versus an unadjusted incidence of 13.7% in patients observed non-operatively for a mean follow-up of 52.5 months, according to Carolyn D. Seib MD, MAS, of Stanford University School of Medicine in California, and co-authors.
On multivariable analysis, parathyroidectomy was associated with lower adjusted rates of any fracture, hip fracture, and adjusted absolute fracture risk reduction at various time points versus non-operative management, they stated in JAMA Internal Medicine.
Seib’s group concluded that “among older adults with PHPT… operative management should be strongly considered in this population to prevent fracture-related morbidity and disability.”
The study joins two others from 2021 by Seib and colleagues: The first, in Surgery, found that most privately insured patients with primary hyperparathyroidism in the U.S. were not treated with parathyroidectomy, and that having an operative indication for the procedure only modestly increased its likelihood; the second, in JAMA Surgery, reported that older age, frailty, and multiple comorbidities were tied to non-operative management of PHPT in older Medicare beneficiaries. In addition, “guideline recommendations had minimal effect on treatment decisions,” Seib’s group noted.
What are those guidelines? The NIH Fourth International Workshop put out a 2014 consensus statement that acknowledged that the procedure had benefits— “even in these subjects who don’t meet any criteria for parathyroidectomy, surgery is always an option because it is the only definitive therapy for PHPT,” they wrote—but also called for more research on parathyroidectomy and fracture incidence before and after surgery, as well as “neurocognitive and vascular function before and after parathyroidectomy.”
The American Association of Endocrine Surgeons (AAES) released recommendations in 2016 in favor of the procedure, stating that “parathyroidectomy is indicated for all symptomatic patients, should be considered for most asymptomatic patients, and is more cost-effective than observation or pharmacologic therapy.”
In an editorial accompanying the current study, Anand R. Habib, MD, MPhil, of the University of California San Francisco, and Mitchell H. Katz, MD, of NYC Health + Hospitals in New York City, said the findings from Seib’s group “add to the growing need to reexamine the 2014 National Institutes of Health consensus recommendations for patients for whom parathyroidectomy should be considered upfront.”
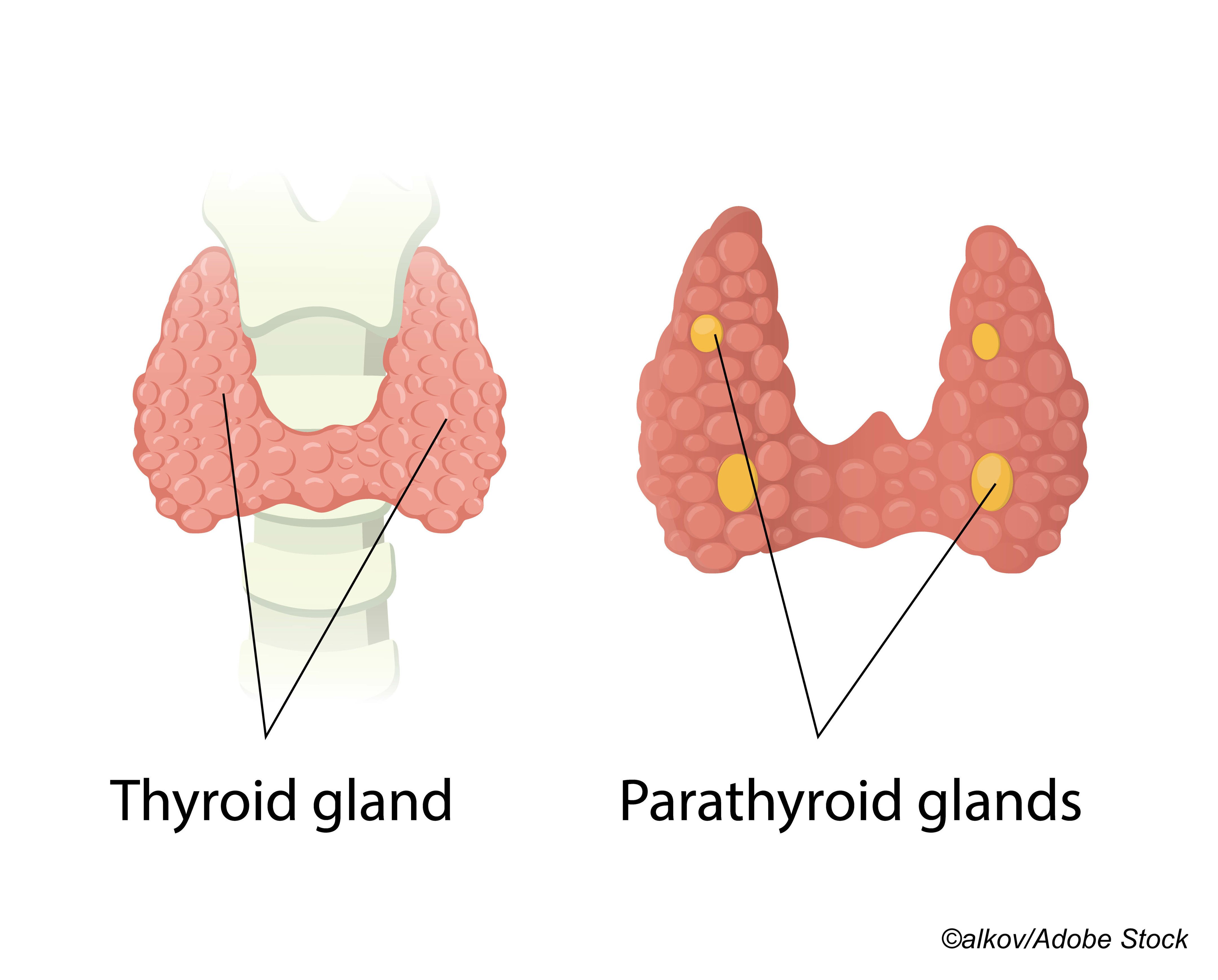
After all, PHPT is the most common cause of chronic hypercalcemia, and increases in incidence for both sexes with advancing age, they explained. While about 80% of these patients initially lack symptoms such as nephrolithiasis, kidney dysfunction, gastrointestinal upset, and neuropsychiatric effects, PHPT accelerates bone turnover for all patients, predisposing them to osteoporosis and fragility fractures, Habib and Katz emphasized.
“Decisions to pursue surgery should still be based on shared decision-making between patient and physician and consider the potential complications,” they stated. Nonetheless, “the advent of minimally-invasive techniques has lowered the rates of these complications, and cure rates of 95% to 99% have been reported,” per the AAES guidelines. A 2021 study out of South Korea detailed ways to select the optimal parathyroidectomy methods for PHPT.
The current authors built multivariable, inverse probability weighted Cox proportional hazards and Fine-Gray competing risk regression models, and applied them to 210,206 Medicare beneficiaries, from 2006 to 2017, who diagnosed with PHPT as identified by ICD-9 or ICD-10 diagnosis codes.
The cohort (mean age 75; 78.8% women; 87.3% White) consisted of two arms: 30% of the patients were treated with parathyroidectomy within 1 year of PHPT diagnosis and 70% who were managed non-operatively, and that group included those who got delayed parathyroidectomy.
The researchers noted that patients treated with parathyroidectomy were younger compared with the nonoperative group (mean age 73.5 vs 76, P<0.001), and more likely to be White, not frail, and a have a lower comorbidity burden. They were also less likely to have a have history of osteoporosis and prior fracture.
The primary outcome was clinical fracture at any anatomic site not associated with major trauma during the follow-up period. The secondary outcome of interest was incident clinical hip fracture.
Seib and co-authors reported that parathyroidectomy versus non-operative management was tied to an adjusted absolute fracture risk reduction of:
- 1.2% (95% CI 1.0 to 1.4) at 2 years.
- 2.8% (95% CI 2.5 to 3.1) at 5 years.
- 5.1% (95% CI 4.6 to 5.5) at 10 years.
They also found that Fine-Gray competing risk regression confirmed parathyroidectomy was associated with a lower probability of any fracture and hip fracture when accounting for the competing risk of death (hazard ratio 0.84, 95% CI 0.82 to 0.85; HR 0.83, 95% CI 0.80 to 0.85, respectively).
On subgroup analysis, the authors found “no significant differences in the association of parathyroidectomy with fracture risk among women of postmenopausal age and older men, those individuals with and without osteoporosis, or those who met and did not meet operative guidelines, suggesting the skeletal benefits of parathyroidectomy are not limited to specific populations at higher risk of fractures.”
As for harms linked with parathyroidectomy, which were assessed by relevant ICD codes within 6 months of surgery, Seib’s group reported that recurrent laryngeal nerve injury was the primary one, but only occurred in 0.99% (n=622/63,136 patients).
Study limitations included the use of administrative claims data for analysis that lacked detailed clinical information about PHPT or associated metabolic complications. Also, they include patients who underwent delayed parathyroidectomy in the non-operative group to “mimic” an intention-to-treat analysis and reduce treatment selection bias so “[l]arger benefits of parathyroidectomy would have been observed in an as-treated analysis.”
-
Parathyroidectomy was associated with a lower adjusted risk of any clinical fracture and hip fracture compared with nonoperative management in older adults with primary hyperparathroidism (PHPT).
-
There were no significant differences in the association of parathyroidectomy with fracture risk by age group, sex, frailty, history of osteoporosis, or meeting operative guidelines based on subgroup analysis.
Shalmali Pal, Contributing Writer, BreakingMED™
Seib reported support from, and/or relationships with, the National Institute on Aging (NIA), Virtual Incision, iota Biosciences, Medtronic, Prescient Surgical, RPWB, and the American Federation of Aging Research. Co-authors reported support from, and/or relationships with, the NIA, the Claude D. Pepper Older American Independence/NIA/NIH, the University of California San Francisco, and the Department of Veterans Affairs Health Services Research & Development.
Habib reported being an editorial fellow at JAMA Internal Medicine. Mitchell reported serving as JAMA Internal Medicine deputy editor.
Cat ID: 110
Topic ID: 76,110,730,110,187,192,652,925