Post-ischemic stroke cognitive impairment is common and related to infarct location, a pooled data analysis showed.
About 44% of 2,950 participants with ischemic stroke had post-stroke cognitive impairment, which was strongly associated with infarcts in the left frontotemporal lobes, left thalamus, and right parietal lobe, reported Geert Jan Biessels, PhD, of the University Medical College of Utrecht in the Netherlands and co-authors in Lancet Neurology.
“80% or more of patients with infarcts in these regions had [post-stroke cognitive impairment],” the researchers wrote. “Building on the historical notion that infarct location determines cognitive impairment, we have now established which locations are most strongly predictive of post-stroke cognitive impairment across most of the brain.”
“We provide an easy-to-use visual rating scale that can be applied by clinicians to identify patients at risk,” they added. “This scale could facilitate cognitive prognostication, help to identify patients who should undergo cognitive assessment, and allow for timely intervention with rehabilitative treatment strategies.”
The group pooled 12 patient cohorts identified through January 2019 in the Meta VCI Map consortium data index to form their sample (mean age about 67, 39% women). All patients had imaging demonstrating acute infarct (median 4 days after index event) and were in studies that included cognitive assessment within 15 months of the index stroke with either a neuropsychological assessment (79.4%) or the Montreal Cognitive Assessment (MoCA; 20.6%). Median time to cognitive assessment was 105 days.
Across the 12 cohorts, post-stroke cognitive impairment was seen more frequently in people with neuropsychological testing (range 18.1%-62.3%) than with MoCA (2.7%-20.5%).
In an accompanying editorial, Leonardo Pantoni, MD, PhD, of the University of Milan, and Emilia Salvadori, PhD, of the University of Florence, both in Italy, wrote that the study “is a substantial contribution in advancing current knowledge around the relevance of lesion location for post-stroke cognitive impairment.”
“However, other potential early predictors should be also considered,” the editorialists noted. “For example, a brief cognitive examination in the stroke unit in the acute phase after the event can predict a medium term diagnosis of cognitive impairment and at low cost.”
“These findings also need to be viewed in the context of therapeutic approaches,” they added. “For example, should a patient with a brain infarct at a specific location and, perhaps, cognitive impairment according to an evaluation in the acute phase of stroke receive a different therapeutic and rehabilitation approach than a patient who does not have these characteristics? This question will need to be addressed in future studies to reduce the large burden associated with the long-term cognitive consequences of stroke.”
Appreciation for non-motor aspects of stroke injury and recovery has grown over the last two decades. A 2009 report showed up to half of stroke patients have post-stroke cognitive impairment of some degree when including about 10% with pre-stroke dementia, 10% with newly diagnosed dementia after stroke, and over 30% with dementia after recurrent stroke. This analysis found post-stroke dementia was associated with stroke characteristics rather than risk factors for pre-stroke dementia.
A 2016 study that, like the present work, combined lesion symptom mapping and predictive modeling, identified left frontotemporal, hippocampal, and thalamic areas as predictive of post-stroke cognitive impairment assessed using the MoCA.
Post-stroke cognitive impairment, with mood, fatigue, and other symptoms “are still rarely assessed, and only partly recognized, perhaps because their assessment is demanding in terms of time and can be difficult, if assessors are not prepared to give advice on psychocognitive deficits and their associated emotional strain,” Pantoni and Salvadori observed.
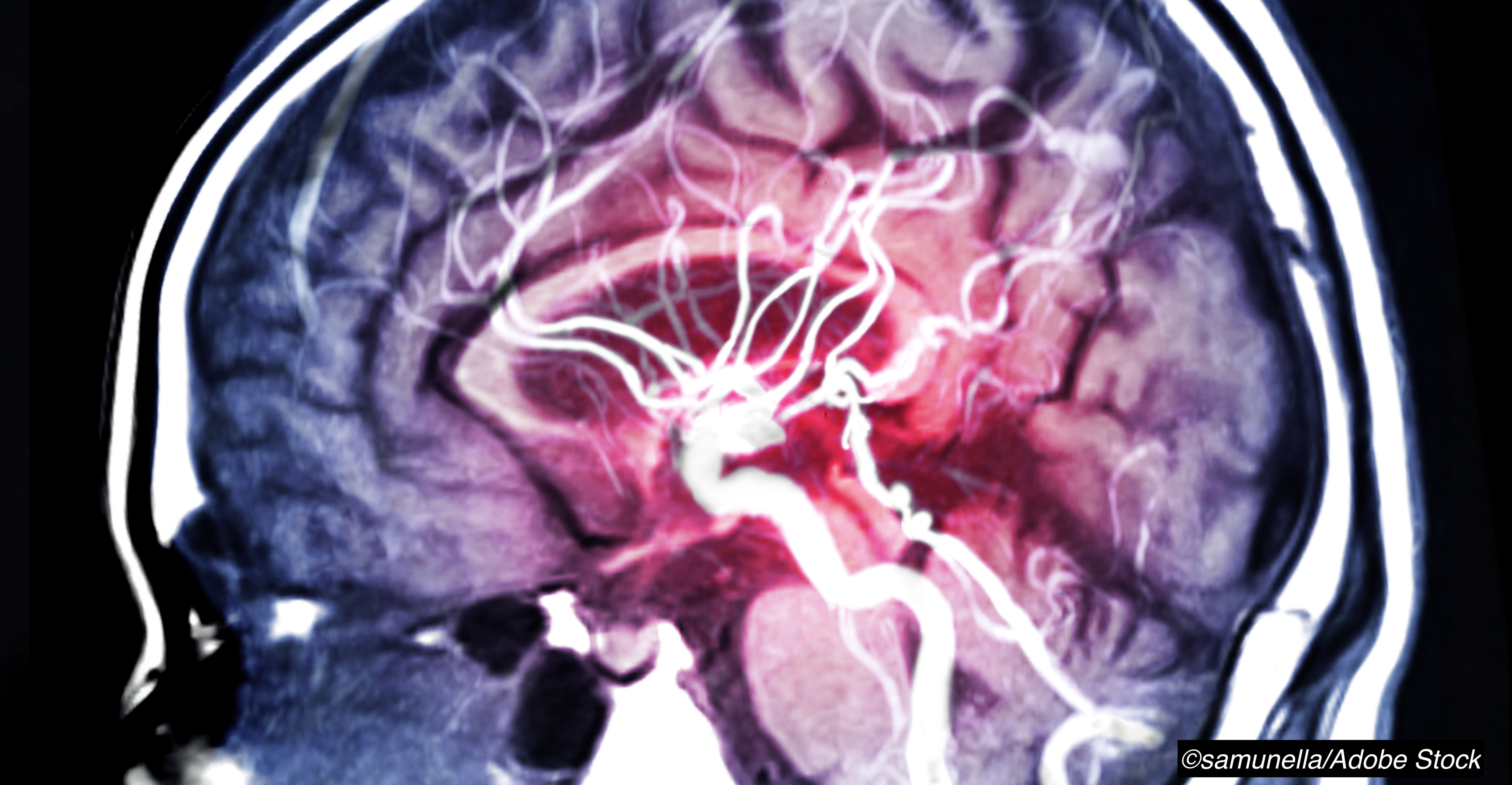
In the present study, Biessels and colleagues defined post-stroke cognitive impairment based on published criteria. They also presented a five-point lesion impact score relating an individual’s infarct location to post-stroke cognitive impairment risk using voxel-based lesion-symptom mapping. Voxels damaged in five or more patients were included in the analysis, and the resulting map covered 87% of the available voxels in 1-mm thick template used.
With P<0.05 for all point values, they cited the predicted probability of post-stroke cognitive impairment ranging from 30% (1 point, 0-20th percentile) to 66% (5 points, 80-100th percentile).
The score, visually determined based on color-coded image maps, is “the first prediction tool for post-stroke cognitive impairment based solely on clinically available brain images,” they wrote. “Although awaiting further testing in prospective studies, the score appears promising for direct application in clinical practice for cognitive prognostication.”
“When interpreting our findings, it is important to consider that infarct locations predictive of post-stroke cognitive impairment do not necessarily imply causality,” the researchers noted. “Confounding factors such as the interdependency between infarct locations (i.e., infarct patterns are not random but follow the vascular tree), clinical history (e.g., pre-stroke cognition, depression), and other brain lesions (e.g., white matter hyperintensities, previous infarcts) should be taken into account.”
Limitations of the study include an include absence of uniform operationalized criteria for post-stroke cognitive impairment. In addition, the time to cognitive assessment after stroke was variable.
-
Post-ischemic stroke cognitive impairment is common and related to infarct location, a pooled data analysis showed.
-
About 44% of ischemic stroke patients had post-stroke cognitive impairment strongly associated with infarcts in the left frontotemporal lobes, left thalamus, and right parietal lobe.
Paul Smyth, MD, Contributing Writer, BreakingMED™
Funding for the study was provided by the Netherlands Organization for Health Research and Development.
Biessels reported grants from the Netherlands Organization for Health Research and Development (ZonMW) during the conduct of the study.
Pantoni has been a member of the European Stroke Organization dementia committee and of the European Stroke Organization panel for defining guidelines for covert cerebral small vessel disease. Salvadori declared no competing interests.
Cat ID: 361
Topic ID: 82,361,730,361,38,748,192,925