1. In patients with a pancreatic or periampullary tumour undergoing pancreaticoduodenectomy (PD), this retrospective study found no difference in surgical complications in patients who underwent preoperative biliary draining (PBD) and patients who did not undergo PBD.
2. Bilirubin level >15 mg/dL in patients undergoing PD was correlated with significantly higher overall complications.
Evidence Rating Level: 2 (Good)
A significant complication of pancreatic and periampullary tumours is biliary obstruction, which can lead to cholangitis, coagulopathies, and gastrointestinal symptoms. The standard procedure for resecting these tumours is a pancreaticoduodenectomy (PD), which is associated with high mortality and morbidity. Hyperbilirubinemia was hypothesized to negatively affect the outcome following PD; addressing biliary obstruction with preoperative biliary drainage (PBD) was thought to reduce post-operative complications. However, there has been limited evidence regarding this, and the latest guidelines suggest the use of PBD according to certain criteria. This retrospective study included patients who underwent PD in three medium-volume Iranian centers between September 2012 and February 2022. Patients were further divided into two populations based on biliary obstruction, defined as a report of subjective jaundice or total bilirubin level of >2 mg/dL. With respect to the management of jaundice, most patients underwent endoscopic retrograde cholangiopancreatography (ERCP) and stent placement prior to referral to a pancreatic surgeon, and in cases of unsuccessful ERCP, a percutaneous transhepatic catheter (PTC) was used. During the study period, PD was performed by a total of 12 surgeons with similar techniques. Outcomes included mortality, defined as death within 90 days after surgery, severe post-operative primary surgical complications, as well as secondary surgical complications such as delayed gastric emptying (DGE), postoperative hemorrhage, postoperative pancreatic fistula (POPF), intraabdominal abscess, and wound infection. 147 patients were included in the study, with 73 (49.7%) receiving preoperative biliary stenting. Postoperatively, overall morbidity was 40.7% and mortality was 21.1%. There was no significant difference in postoperative mortality and morbidity between patients who received PBD and patients who did not receive PBD. Interestingly, bilirubin >15 mg/dL was correlated with higher overall complications (63.6% vs 33.0%, p=.008). In addition, surgery duration was significantly longer in patients with wound infection, intra-abdominal abscess, DGE, secondary complications, and overall complications. Of note, in patients with biliary obstruction, postoperative morbidity and mortality were similar between the PBD and no PBD group, with no risk factors significantly impacting outcomes. Overall, the findings from this study suggest no difference between PBD and no PBD in patients undergoing PD for pancreatic and periampullary tumours. A limitation of this study was that it was conducted only in Iran, and the results may not be generalized to populations with differing racial profiles. This study is an addition to the growing body of evidence surrounding preoperative biliary stenting; it is important to consider the potential financial burden of PBD and possible complications in the absence of clear benefits of the intervention.
Click to read the study in BMC Surgery
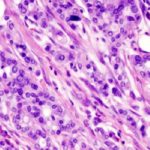
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.