Among women treated for symptomatic uterine fibroids, myomectomy was associated with better quality of life than uterine-artery embolization 2-years later in the randomized FEMME trial, which compared the two fertility-sparing therapeutic strategies.
In addition to significantly better quality of life, the multicenter study, which enrolled 254 premenopausal women, found that treatment with myomectomy was associated with lower severity of symptoms such as heavy menstrual bleeding, abdominal pain, and subfertility.
Both procedures were associated with significant improvements in quality of life over baseline, however, and pregnancy rates were similar, but low, at year 2-9 pregnancies and 6 live births following embolization versus 5 pregnancies and 4 live births following myomectomy.
The overall incidence of perioperative and postoperative complications was also similar in the two groups.
The study findings were published online July 29 in New England Journal of Medicine.
“The overall incidence of complications associated with both procedures was low,” wrote researcher Isaac Manyonda, PhD, of St George’s Hospital and Medical School, London, and colleagues.
They noted that additional procedures were performed in 7% of the women randomized to the myomectomy arm of the trial, compared with 16% in the uterine-artery embolization, and that the median length of hospital stay was 4 days with myomectomy and 2 days with uterine-artery embolization.
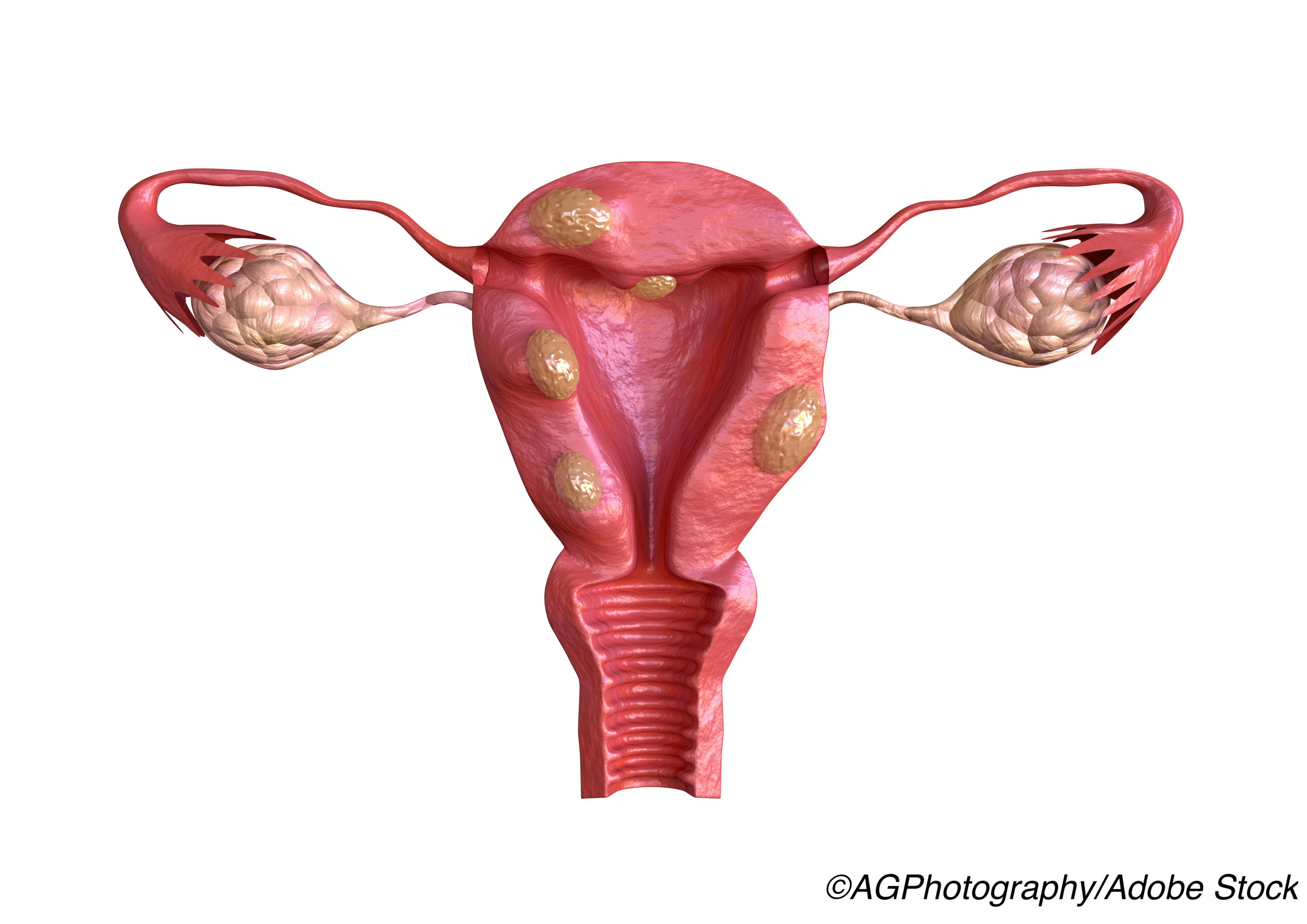
Hysterectomy remains the main treatment for symptomatic uterine fibroids, with uterine-sparing myomectomy routinely offered to premenopausal women in cases where preserving fertility is desired.
Uterine-artery embolization emerged as an alternative to surgical treatment in the 1990s. Often performed under local anesthesia, the procedure involves the use of biocompatible particles to block the arteries supplying the uterus, leading to ischemic infarction of fibroids.
“As compared with myomectomy, uterine-artery embolization is associated with a shorter hospital stay and an earlier return to normal activities, but also a higher likelihood of the need for additional intervention,” the researchers wrote.
“Concern regarding a possible effect on ovarian and uterine function has resulted in recommendations against the use of uterine-artery embolization in women who plan to become pregnant; however, the results of a recent meta-analysis suggested no appreciable effect on ovarian reserve.”
The meta-analysis found no evidence that uterine artery embolization impacted ovarian reserve, as measured by serum concentrations of anti-Mullerian hormone (AMH) and follicle stimulating hormone (FSH).
The multicenter, open-label FEMME trial was performed to compare the two strategies in the treatment of symptomatic uterine fibroids in premenopausal women wishing to avoid hysterectomy. Fibroid-related quality of life was the main outcome measure, assessed using the Uterine Fibroid Symptom and Quality of Life (UFS-QOL) questionnaire, administered 2 years after treatment.
The study participants were recruited from 29 hospitals in the United Kingdom, with 127 women randomly assigned to the myomectomy group and 127 to the uterine-artery embolization group. A total of 105 and 98, respectively, actually underwent myomectomy or the embolization procedure, and 2-year follow-up questionnaire data were available for 206 (81%) women originally randomized.
Among the main study findings:
- The mean (±SD) score on the health-related quality-of-life domain of the UFS-QOL questionnaire at 2 years was 84.6±21.5 in the myomectomy group and 80.0±22.0 in the uterine-artery embolization group (mean adjusted difference with complete case analysis, 8.0 points; 95% CI, 1.8-14.1; P = 0.01; mean adjusted difference with missing response was 6.5 points; 95% CI, 1.1-11.9).
- Perioperative and postoperative complications from all initial procedures, irrespective of adherence to the assigned procedure, occurred in 29% of the women in the myomectomy group and in 24% of the women in the uterine-artery embolization group.
- The most commonly reported complication was infection, occurring in 15 (14%) of the embolization patients and 17 (15%) of the myomectomy patients.
“The incidence of intraoperative complications was low, with only one conversion of a myomectomy to a hysterectomy and one conversion of a laproscopic myomectomy to an open abdominal embolization,” the researchers wrote.
Just 8% of women in the embolization group and 4% of those in the myomectomy group reported a pregnancy within 2 years of receiving treatment, and there were no consistent differences between the two groups in ovarian reserve.
The researchers wrote that “there were too few pregnancies in our trial to inform the effects of the procedures on fertility.”
Study limitations cited by the researchers included the fact that 1 in 5 (19%) study participants failed to return the primary outcome questionnaire at 2-year follow-up and the fact that some women did not receive the assigned treatment.
In an accompanying editorial, Elizabeth A. Stewart, MD, of Mayo Clinic, Rochester, wrote that a major strength of the FEMME study was the diverse population, with Black women making up 38% and 43%, respectively, of the embolization and myomectomy groups.
“This representation is critical, since the risk of fibroids is three times greater among women of African descent than among white women, and the diagnosis of fibroids tends to be earlier and the severity of disease greater among Black women,” she wrote.
Stewart noted that a major reason to compare uterine-artery embolization and myomectomy is to assess reproductive outcomes, given that embolization is not often used in younger women due to concerns about infertility “despite very-low quality evidence to support the superiority of myomectomy with regard to pregnancy outcomes.”
“The FEMME trial is among the first major trials to evaluate alternatives to hysterectomy that included an assessment of the intention for pregnancy and that enrolled women in whom future pregnancy was desired; as such, it is a big step forward,” she wrote.
While the overall prevalence of pregnancy was low in both groups, biomarkers of ovarian reserve were similar.
“These findings set the stage for a larger randomized trial of uterine-artery embolization versus myomectomy, powered to detect live birth rates,” Stewart wrote, adding that the low pregnancy rate may have been influenced by the fact that the average age of the trial participants was greater than 40 years.
She wrote that the FEMME trial “provides new data on outcomes that differ from previously published literature in which uterine-artery embolization was compared with hysterectomy.”
“Trials comparing outcomes among uterine-sparing treatments should be undertaken to give women and their providers the data they need to make key decisions about these alternatives to hysterectomy,” she concluded.
-
Among women treated for symptomatic uterine fibroids, myomectomy was associated with better quality of life than uterine-artery embolization 2-years later.
-
Both procedures were associated with significant improvements in quality of life over baseline, and pregnancy rates were low, but similar, with the two treatments.
Salynn Boyles, Contributing Writer, BreakingMED™
Manyonda had no disclosures.
Stewart reported personal fees from Bayer, personal fees from AbbVie, personal fees from Myovant, personal fees from UpToDate, personal fees from Med Learning Group, personal fees from PeerView, personal fees from ObsEva, outside the submitted work; In addition, Stewart has a patent Methods and Compounds for Treatment of Abnormal Uterine Bleeding ( US 6440445) issued.
Cat ID: 133
Topic ID: 83,133,730,133,191,192,925