A team of pediatric oncologists and cancer researchers from Tokyo’s National Cancer Center Hospital say they have confirmed the transmission of cervical cancer tumors from pregnant women to the lungs of their children.
“Two cases of pediatric lung cancer (in 23-month-old and 6-year-old boys) resulting from mother-to-infant transmission of uterine cervical tumors were incidentally detected during routine next-generation sequencing of paired samples of tumor and normal tissue,” wrote Ayumu Arakawa, MD, and colleagues in a brief report in The New England Journal of Medicine. “Spontaneous regression of some lesions in the first child and slow growth of the tumor mass in the second child suggested the existence of alloimmune responses against the transmitted tumors. Immune checkpoint inhibitor therapy with nivolumab led to a strong regression of all remaining tumors in the first child.”
The possibility of such transmission was previously established, but it is extremely rare, estimated at 1 case of such transmission in every 500,000 pregnant women with cancer. Previously reported cases occurred among women with cervical cancer, as well as cancers of the blood or skin cancers. In those cases, the cancer was believed to be transmitted “hematogenously (through transplacental mother-to-fetus transmission) and often involved dissemination of maternal tumor cells to multiple organs (e.g., brain, bone, liver, and soft tissues) in the infant, Arakawa and colleagues explained. “All the reported cases were diagnosed in children younger than 2 years of age.”
The researchers performed the cancer sequencing as part of a prospective clinical trial in pediatric cancer patients. “We used a next-generation sequencing–based solid-tumor test in which germline DNA was used as a control. This National Cancer Center Oncopanel test is a hybridization capture–based next-generation sequencing assay,” they wrote.
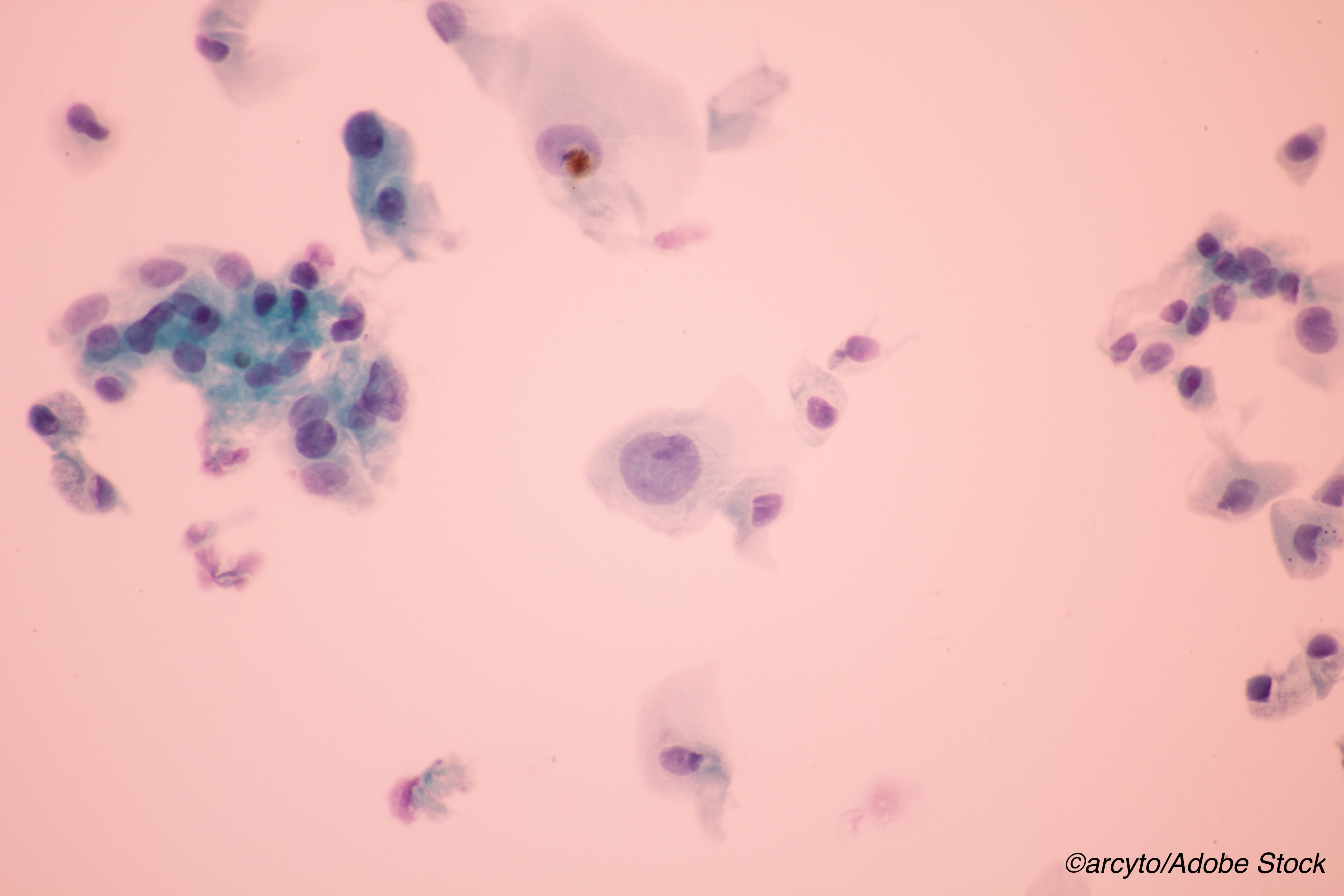
The 23-month-old child—a boy—had a 2-week history of productive cough. He underwent imaging with computed tomography, which revealed multiple masses in both lungs. Biopsy confirmed neuroendocrine carcinoma of the lung with focal glandular differentiation.
A review of the mother’s records revealed that cervical cytologic testing early in her pregnancy was negative and the child was delivered transvaginally at 35 weeks.
“The 35-year-old mother, who had not received vaccination against human papillomavirus (HPV), received a diagnosis of squamous-cell carcinoma of the cervix 3 months after the infant’s birth,” Arakawa and colleagues noted. “After the diagnosis, she underwent radical hysterectomy with pelvic lymphadenectomy, followed by four cycles of adjuvant chemotherapy. At that time, transmission of the tumor to her son was not suspected because the histologic characteristics were thought to be different from those of her son.”
The boy’s parents did not want immediate treatment, but he was followed closely for a year, at which time some of his tumors had progressed.
Arakawa and colleagues wrote that the boy was referred to their hospital for treatment at age 3.
“Surprisingly, some of the lesions had spontaneously regressed by that time,” they wrote. “However, round opacities on radiographic images indicated that multiple foci of the tumor were still present in both lungs. CT imaging confirmed that tumor masses were spread along the bronchi. The patient received five cycles of chemotherapy with cisplatin (at a dose of 60 mg per square meter of body-surface area on day 1) and irinotecan (60 mg per square meter on days 1, 8, and 15 of each 28-day cycle), followed by two cycles of carboplatin (400 mg per square meter on day 1 and 2) and etoposide (100 mg per square meter on days 1 to 5 of each 28-day cycle). Some of the tumors shrank, but others subsequently progressed.”
During this time, the mother’s cancer had also progressed, with metastases in lung, liver, and bone. “Pathological reexamination of the hysterectomy specimen revealed that the cervical cancer was predominantly poorly differentiated squamous-cell carcinoma with focal neuroendocrine differentiation admixed with a minor component of adenocarcinoma; this histologic picture was similar to the tumor in her lung as well as that in her son’s lung,” they wrote.
At that point, genetic testing on both the boy’s tumors and the mother’s tumors confirmed that both tumors had the “same pathogenic KRAS (c.G38A:p.G13D) and TP53 (c.G853A:p.E285K) mutations, and 47 exonic single-nucleotide polymorphism (SNP) alleles carried by the mother but not inherited in the child’s germline were detected in the child’s tumor (i.e., the child’s tumor was related to the mother’s tumor and contained genes that were not in the child’s germline genome).”
The boy’s cancer progressed on chemotherapy, so he was enrolled in a trial of nivolumab at a dose of 3 mg per kilogram every 2 weeks. He underwent 14 cycles of nivolumab, responded to therapy, and had remaining nodules resected. ’The patient had no evidence of disease recurrence at 12 months after lobectomy,” they wrote.
The mother was enrolled in another nivolumab trial but did not respond to treatment. She died after disease progression.
The other case of mother-to-child transmission, involved a 6 year-old boy who presented with left-side chest pain. Imaging revealed a 6-cm in diameter mass in the lung and he was diagnosed with mucinous adenocarcinoma.
The researchers did not initially suspect maternal transmission in this case, although the mother was known to have a cervical polypoid tumor present during pregnancy. As was the case with mother of “patient 1,” cervical cytology for this woman was also negative during pregnancy. She delivered her son vaginally at 38 weeks. “Biopsy of the cervical lesion after the delivery revealed adenocarcinoma, and she was referred to a university hospital for radical hysterectomy and bilateral salpingo-oophorectomy 3 months after delivery. She died of the disease 2 years after the surgery,” the researchers wrote.
The boy’s tumor was inoperable, so he underwent several chemotherapy cycles with different toxic regimens and eventually underwent pneumonectomy. “Pathological examination of the lung showed mucinous adenocarcinoma, which is an unusual morphologic finding for a primary lung tumor, but it was similar to the uterine cervical tumor in the mother,” they explained. “He was followed for 15 months after pneumonectomy and was free from disease.” Again, DNA sequencing revealed the link between the mother’s tumor and the boy’s cancer.
Of note, in both cases, the tumors in the boys “lacked the Y chromosome and shared multiple somatic mutations, an HPV genome, and SNP alleles (which were not inherited in the children’s germline) with tumors from the mothers.”
Arakawa and colleagues pointed out that “HLA class I alleles, which were not inherited by Patient 1, were lost in the tumors in this child and his mother. This phenomenon has been reported in a case of mother-to-fetus transmission of leukemia cells. Since HLA proteins are known to provide major antigenic targets for allograft recognition and rejection, the loss of HLA alleles might have contributed to the survival of the maternal tumor cells in the child. Patient 1 had spontaneous regression of several lesions within 1 year after detection of the tumor, during the follow-up period when he was not receiving treatment; this regression occurs extremely rarely in metastatic neuroendocrine carcinomas. In addition, the remaining tumors evidently had a response to anti–PD-1 immune checkpoint inhibitor therapy, although neither PD-1 nor PD-L1 was expressed in this patient, and immune checkpoint therapy is known to be ineffective in most solid tumors in children. In contrast, this patient’s mother did not have a response to the same anti–PD-1 therapy. In Patient 2, the tumor grew very slowly, and clinical manifestations did not occur until he was 6 years of age. This slow growth is very rare for metastatic cervical adenocarcinoma; therefore, it appears likely that an alloimmune response in the child affected the rate of tumor growth.”
-
Be aware that this brief report confirms the transmission of cervical cancer tumors from pregnant women to the lungs of their children.
-
Note that although mother-to-child transmission of cancer cells has been previously reported, it is extremely rare and is estimated to occur in only 1 of 500,000 pregnancies in women with cancer.
Peggy Peck, Editor-in-Chief, BreakingMED™
Arakawa disclosed grant support from Astelias Pharma, AstraZeneca, and Chagal Pharmaceutical Co., Ltd.
Cat ID: 120
Topic ID: 78,120,730,120,935,191,41,192,925


