Guillain-Barré syndrome (GBS) patients with a poor prognosis after one course of intravenous immunoglobulin (IVIG) did not benefit from a second course, the randomized SID-GBS trial found.
“A second intravenous immunoglobulin course should not be considered for treatment of Guillain-Barre syndrome because of a poor prognosis,” wrote Pieter van Doorn, MD, of Erasmus MC University Medical Center in the Netherlands, and co-authors, in Lancet Neurology.
“Moreover, it entails a risk of serious adverse events,” they added. “The results indicate the need for treatment trials with other immune modulators in patients severely affected by Guillain-Barré syndrome.”
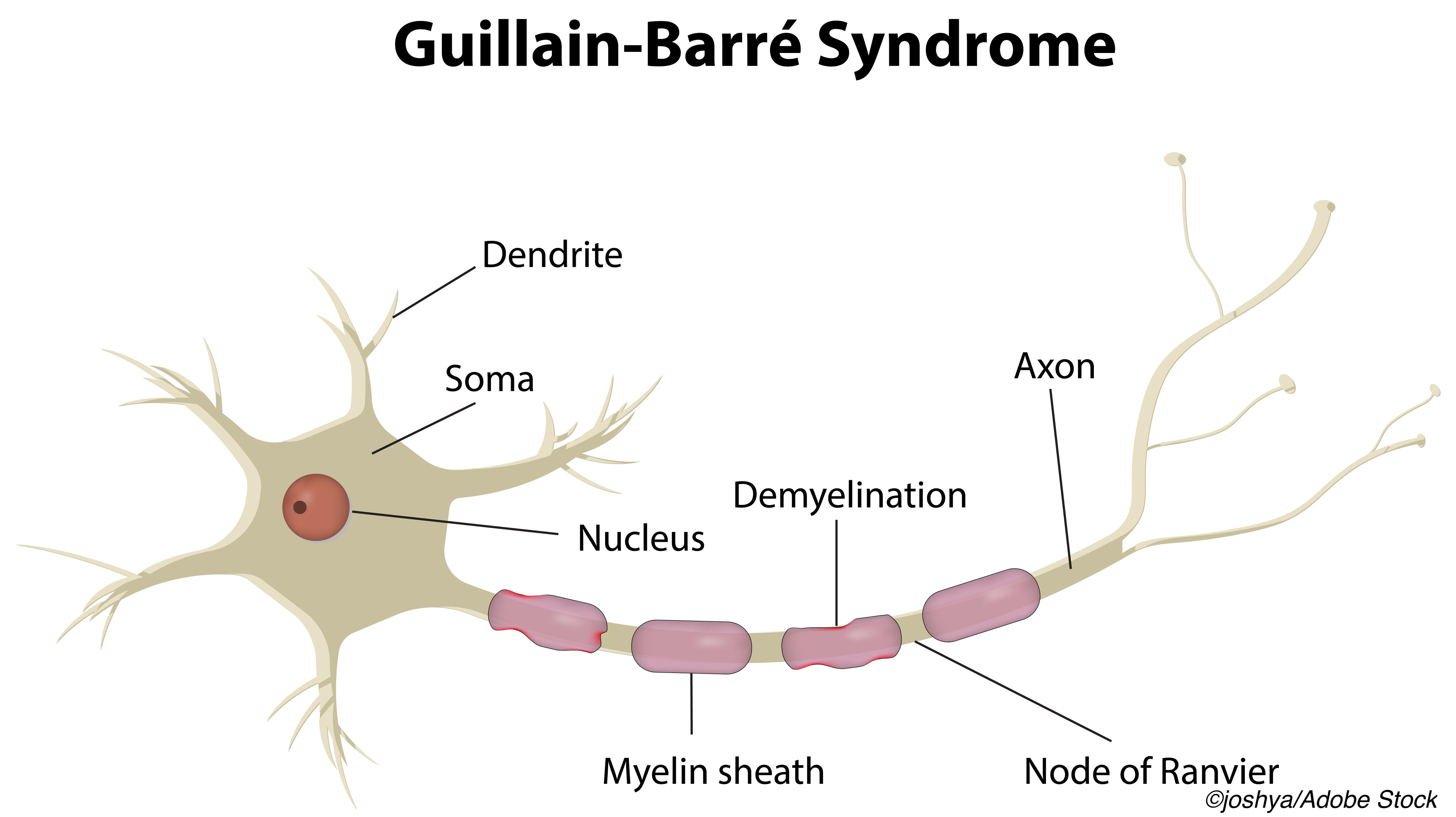
GBS is a post-infectious neuropathy with progressive limb weakness, and variants that affect cranial nerves. The course is often shortened by treatment with IVIG, plasmapheresis and other immune modulators, but up to 20% of patients are unable to walk 6 months after symptom onset and a quarter may experience respiratory insufficiency, with mortality of about 5%.
Investigators included patients 12 or older admitted to a hospital with Guillain-Barré syndrome when they began treatment with a first course of IVIG. Only patients with a score of ≥6 at day 7 on the modified Erasmus Guillain-Barré syndrome outcome score (range 0-12, higher scores indicate worse prognosis) were randomized to a second IVIG dose (n=49) or placebo (n=44). IVIG treatment was given as 2 g/kg over 5 days.
A separate scale, the GBS disability scale (range 0 no symptoms; 6 death) was used to assess the primary outcome at 4 weeks. For patients given a second dose, compared with placebo:
- OR for improvement on the Guillain-Barré syndrome disability score at 4 weeks was 1.4, 95% CI 0.6-3.3, P=0.45
- More serious adverse events were seen in the first 30 days (35% versus 16% for IVIG versus placebo, respectively)
- Four patients died in the intervention group 13-24 weeks after randomization
“Most of us treating Guillain-Barré syndrome for many years have given some second intravenous immunoglobulin doses when we are watching helplessly for the return of limb movement in our patients who are severely affected with the syndrome,”wrote Michael Lunn, MBBS, PhD, of National Hospital for Neurology and Neurosurgery in London, England, in an accompanying editorial. “[This] trial definitively answers the question of whether a second dose has any effect — with the findings suggesting no therapeutic effect for any outcome measure.”
“More importantly, second doses were associated with temporally related harms of clinically significant thromboembolic complications,” he added. “Eventually, appropriate treatment upon presentation through increasing awareness of so-called nerve attack (analogous to widespread brain attack stroke awareness programs) will hopefully improve outcomes. In the interim, we need to stop using our precious intravenous immunoglobulin resource as second doses in severe Guillain-Barré syndrome and concentrate on supporting our patients through sometimes prolonged recovery without inadvertently causing additional harm.”
IVIG is a pooled immunoglobulin product with multiple proposed immune-modulating mechanisms used in autoimmune, infectious, and inflammatory conditions. In addition to concerns about cost and in recent years, availability, a 2018 review of 248 patients treated with IVIG found that only about one-third of those treated were appropriate candidates.
Safety concerns include thrombotic events, with estimated incidence ranging from 1% to about 17%. Risk factors include a large dose, first dose, oral contraceptive use, older age, prior thrombosis, and elevated serum viscosity.
The authors’ earlier observational study comparing one- versus two-course IVIG treatment in patients with GBS and poor prognosis did not show better outcomes after a second IVIG course, but was limited by small numbers and baseline imbalances.
Van Doorn and colleagues conducted the SID-GBS trial between February 2010 and June 2018. Overall 112 patients had an outcome score of 6 or greater. Men made up 63% of the IVIG and 77% of the placebo group. Mean age was 66 for the IVIG group and 59 for the placebo group.
Despite the first course of IVIG in all participants, 85% overall were still deteriorating clinically at 1 week. There were no between group differences in duration of hospital or intensive care stay or duration of mechanical ventilation.
Besides the primary outcome at 4 weeks, GBS disability scores did not differ at weeks 8, 12, or 26, and showed no difference in the likelihood of improving by one or more grades on the disability score at any time point.
Four deaths occurred in the IVIG group: a previously healthy 59-year-old man (acute coronary syndrome 4 days after the second IVIG course); an 82-year-old woman with no improvement and withdrawal of care at 13 weeks; a 72-year-old woman at 21 weeks from cardiac causes; and an 81-year- old woman with no improvement and withdrawal of care at 24 weeks.
Serious adverse events occurred in 51% of the IVIG group and 23% of placebo group, including pneumonia (24% and 16%) and other infection (4% and 2%). Coronary ischemia and renal insufficiency occurred in 2% of both groups. Some events were seen only in the IVIG group, namely, multiple transient ischemic attacks (2%), pulmonary embolism (4%), and radial artery thrombosis (2%).
“Our new approach should be to find treatments that rapidly neutralize the immediate and ongoing damage happening as the patient presents,” the editorialist observed. “A complement inhibitor is an obvious choice. The emerging classes of neonatal Fc receptor inhibitors or IgG metabolizing enzymes, such as imlifidase, might also have potential as treatments.”
Limitations of the study include the absence of direct and indirect costs of giving second IVIG dose in this situation.
-
Guillain-Barré syndrome (GBS) patients with a poor prognosis after one course of intravenous immunoglobulin (IVIG) did not benefit from a second course, the randomized SID-GBS trial showed.
-
Second doses of IVIG were associated with serious adverse events and should not be considered for these patients, the researchers said.
Paul Smyth, MD, Contributing Writer, BreakingMED™
This study was funded by Prinses Beatrix Spierfonds and Sanquin Plasma Products.
van Doorn reports grants from Sanquin Blood Supply and Prinses Beatrix Spierfonds, during the conduct of the study; and grants from Grifols, Takeda, Annexion, Argenx, Commonwealth Serum Laboratories, Octapharma, and Hansa, outside the submitted work.
Lunn reports personal consulting fees for trial development from UCB Pharma, CSL Behring, and Polyneuron, and has received fees from Octapharma, UMC Amsterdam (IoC trial), and AstraZeneca. He is a member of the NHS England IVIG Guidelines and Monitoring Committee.
Cat ID: 130
Topic ID: 82,130,730,130,192,925


