A four-month treatment course that included rifapentine and moxifloxacin was found to be noninferior to the standard six-month tuberculosis treatment regimen in patients with drug-susceptible disease in a phase III, open-label, clinical trial.
The shorter treatment involving 1,200 mg daily doses of rifapentine and 400 mg daily doses of moxifloxacin with isoniazid and pyrazinamide showed similar 12-month tuberculosis-free survival as the standard six months of multidrug therapy involving rifampin.
Rifapentine is a cyclopentyl derivative of rifampin, which has activity against Mycobacterium tuberculosis with a longer half-life.
Moxifloxacin is a fluoroquinolone with activity against M. tuberculosis, which has been shown to accelerate sputum-culture conversion to negative status earlier in the course of treatment when added to first-line antibiotics.
Based on studies in mice showing a rifapentine-moxifloxacin-containing regimen to be associated sustained clearance of M. tuberculosis after three months of treatment, researchers designed a phase III clinical trial to determine whether adding the combination to firstline drugs could reliably shorten treatment in humans.
“Noninferiority of the rifapentine-moxifloxacin regimen to the control regimen was confirmed across analysis populations as well as in sensitivity and prespecified subgroup analyses,” wrote researcher Susan Dorman, MD, of the University of California, San Francisco, and colleagues in New England Journal of Medicine.
A four-month treatment regimen that included rifapentine without moxifloxacin did not meet the criteria for efficacy noninferiority.
The rifapentine-moxifloxacin regimen included eight weeks of once-daily rifapentine (1200 mg), isoniazid, pyrazinamide and moxifloxacin (400 mg) followed by nine weeks of once daily rifapentine, isoniazid, and moxifloxacin.
The standard (control) regimen involved eight weeks of once daily rifampin, isoniazid, pyrazinamide and ethambutol followed by 18 weeks of once-daily rifampin and isoniazid.
A third treatment arm included daily rifapentine, isoniazid, pyrazinamide and ethambutol given for eight weeks, followed by nine weeks of once-daily rifapentine and isoniazid.
Neither the participants nor staff were blinded to the treatment, due to the need to time rifapentine dosing within an hour of eating to maximize drug absorption. In addition, the researchers noted that adding a placebo to treatment would have increased the number of daily pill to approximately 20.
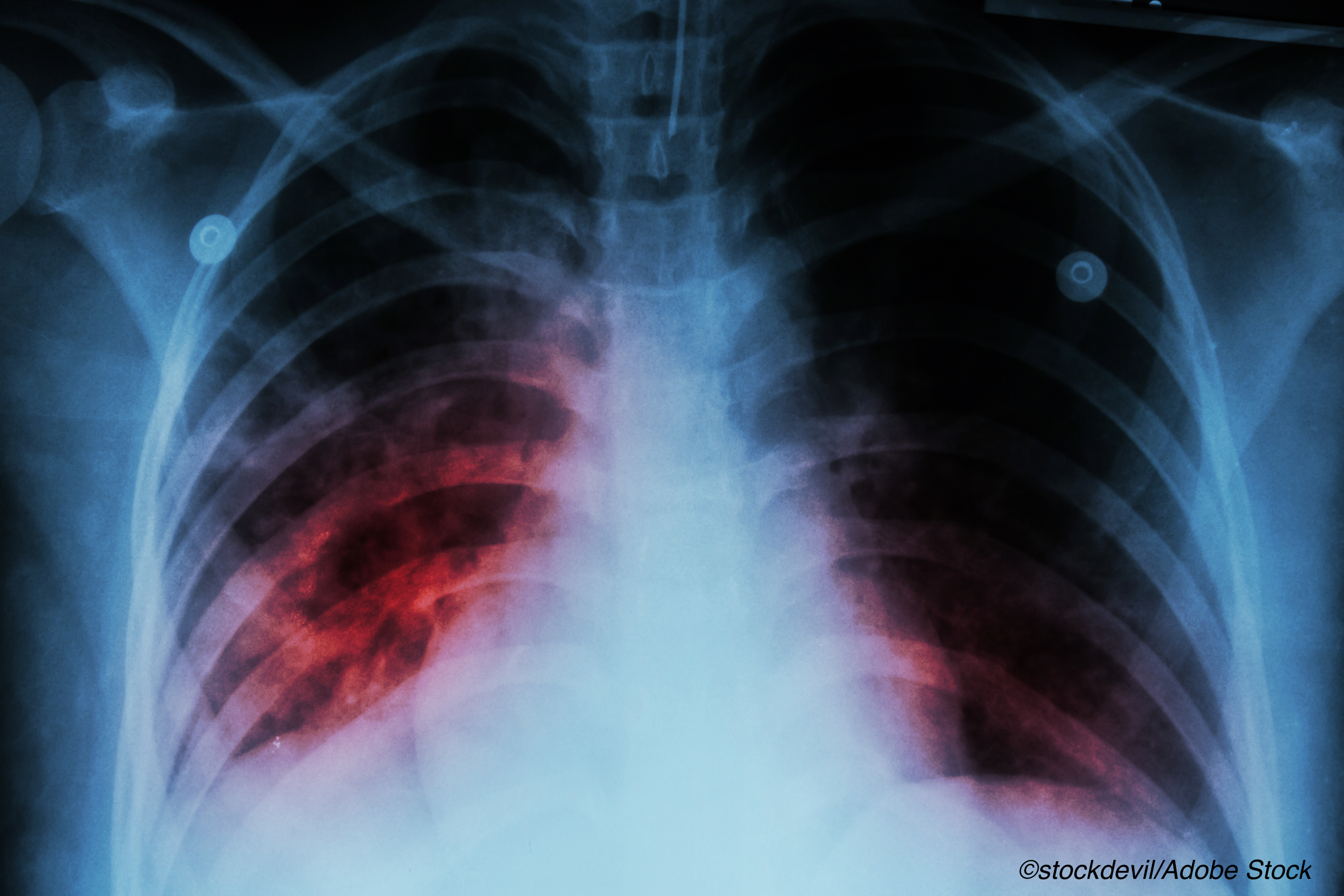
A total of 2,343 patients who underwent randomization for the study had a culture positive for M. tuberculosis that was not resistant to isoniazid, rifampin or fluoroquinolones. The study participants were randomized 1:1:1 to one of the three treatment arms. A total of 194 were co-infected with HIV and roughly 1,700 had cavitation on chest radiography.
A total of 2,234 participants could be assessed for the primary outcome (accessible population; 726 in the control group, 756 in the rifapentine-moxifloxacin group and 752 in the rifapentine group.
Among the main findings:
- Rifapentine with moxifloxacin was noninferior to the control in the microbiologically eligible population (15.5% vs. 14.6% had an unfavorable outcome; difference, 1.0 percentage point; 95% CI, −2.6 to 4.5) and in the assessable population (11.6% vs. 9.6%; difference 2 percentage points; 95% CI, −1.1 to 5.1). Noninferiority was shown in the secondary and sensitivity analyses.
- Rifapentine without moxifloxacin was not shown to be non-inferior to the control in either population (17.7% vs. 14.6% with an unfavorable outcome in the microbiologically eligible population; difference, 3 percentage points (95% CI, −0.6 to 6.6); and 14.2% vs. 9.6% in the assessable population; difference, 4.4 percentage points (95% CI, 1.2 to 7.7).
- Adverse events of grade 3 or greater occurred during the on-treatment period in 19.3% of participants in the control group, 18.8% of those in the rifapentine-moxifloxacin group and 14.3% of those in the rifapentine group.
In an editorial published with the study, NEJM editor-in chief Eric J. Rubin, MD, of Brigham and Women’s Hospital, Boston, and Valerie Mizrahi, PhD, of the University of Cape Town in South Africa wrote that many efforts have been made over the years to shorten the standard 6 month multidrug treatment period for M. tuberculosis.
“There is good evidence that this may be possible, because most patients who receive standard therapy are cured well before 6 months,” they wrote. “The longer duration is driven by a minority of patients for whom extended therapy is warranted. A ’stratified medicine’ approach proposed recently would entail identifying those in need of longer treatment. The alternative approach is to replace the standard regimen with one that provides a durable cure for all patients in less time.”
They noted, however, that several recent large studies of fluoroquinolone-based regimens failed to show noninferiority with a shortened (4 month) treatment regimen.
They added that the findings by Dorman and colleagues have both “immediate and longer-term applications,” adding that questions remain about the treatmen, including whether having to time rifapentine to food intake to maximize absorption could result in new adherence issues.
“Moreover, one of the advantages of the currently used tuberculosis drugs is that they are not widely used in other infections,” they wrote. “In addition to necessitating rapid drug susceptibility testing for moxifloxacin, widespread use of this antibiotic for the treatment of tuberculosis could promote resistance to fluoroquinolones in other bacteria.”
They concluded that the trial established “an important principle: there is no magic with 6 months of therapy,” and they further noted that other novel regimens have recently shown even better efficacy against M. tuberculosis in mice than the rifapentine-moxifloxacin regimen.
“Thus, this trial not only proves that we can have a shorter short-course treatment but also suggests that an even shorter short-course treatment might one day be feasible,” they wrote.
-
A four-month treatment course that included rifapentine and moxifloxacin was found to be noninferior to the standard six-month tuberculosis treatment regimen in patients with drug-susceptible disease in a phase III, open-label, clinical trial
-
The shorter treatment involving rifapentine and moxifloxacin with isoniazid and pyrazinamide showed similar 12-month tuberculosis-free survival as the standard six months of multidrug therapy involving rifampin.
Salynn Boyles, Contributing Writer, BreakingMED™
The study was supported by the CDC; the Division of Tuberculosis Elimination, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention; and the National Institute of Allergy and Infectious Diseases of the National Institutes of Health. Sanofi donated rifapentine and all other trial drugs, supported the shipment of the trial drugs to all sites, and provided funding support for pharmacokinetic testing and preparation of the final clinical study report.
Dorman reported no potential conflicts of interest.
Rubin is Editor-in-Chief of the New England Journal of Medicine.
Mizrahi reported grants and fees from the Bill & Melinda Gates Foundation, outside the submitted work.
Cat ID: 195
Topic ID: 89,195,730,190,310,192,195,311,925



Create Post
Twitter/X Preview
Logout