When choosing between bariatric procedures, sleeve gastrectomy may be a safer bet than Roux-en-Y gastric bypass, with better 5-year outcomes for long-term mortality, complications, and reinterventions—however, patients undergoing the procedure were also more likely to need surgical revision.
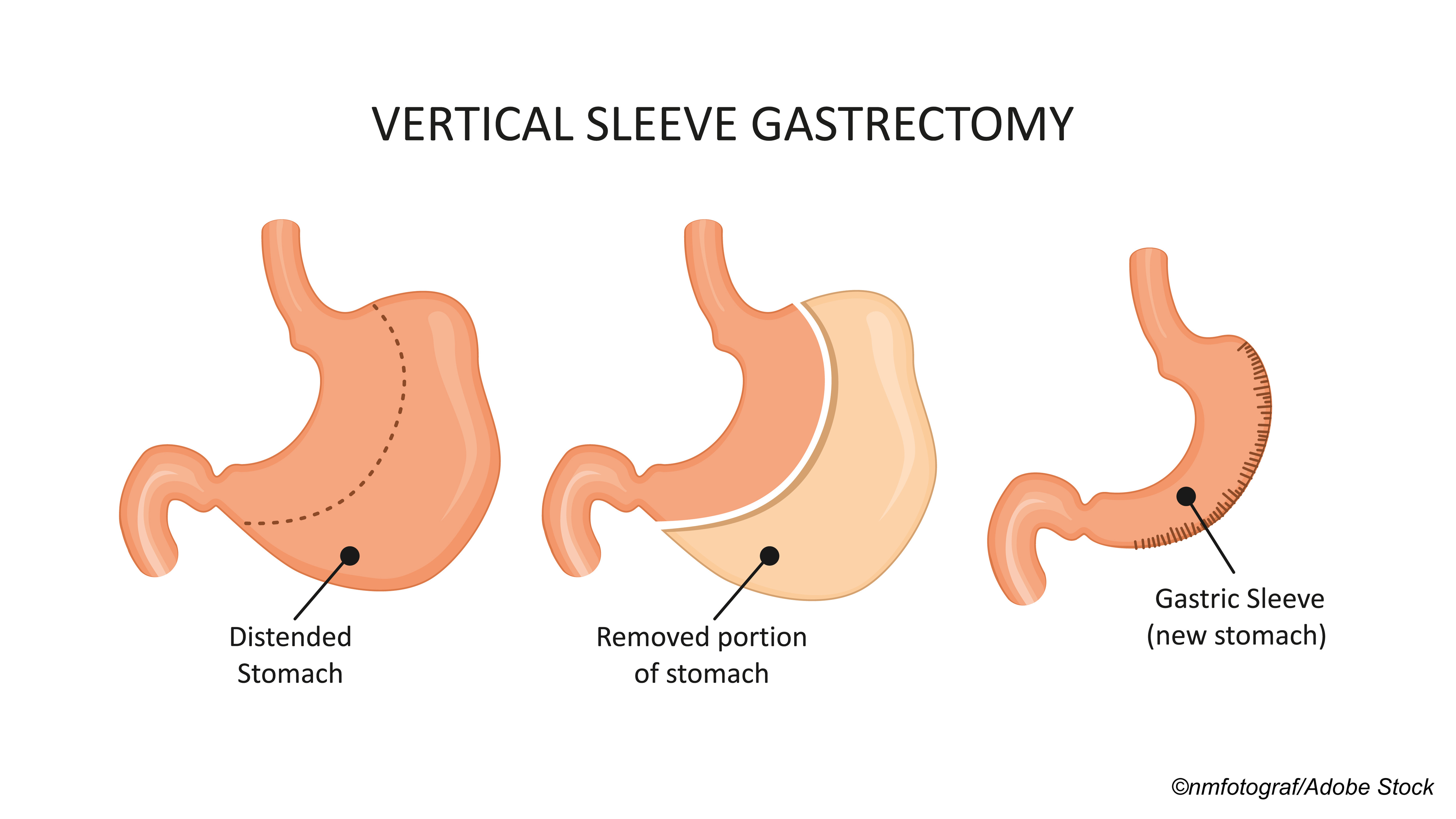
In recent years, sleeve gastrectomy’s good short-term safety profile, effective weight reduction and comorbidity resolution, and technical ease have allowed the procedure to eclipse gastric bypass as the most commonly performed bariatric surgery in the U.S., though bypass follows close behind in the number two spot.
The problem, explained Ryan Howard, MD, of the University of Michigan in Ann Arbor, and colleagues, is that the long-term safety of sleeve gastrectomy versus gastric bypass is not well known. And, notably, while CMS covers both procedures for Medicare Beneficiaries, the Medicare Evidence Development and Coverage Advisory Committee “has expressed low confidence in existing evidence for bariatric surgery” due to a lack of long-term data in this population, they wrote in JAMA Surgery.
In order to better illustrate the long-term safety profile of bariatric surgeries, Howard and colleagues conducted a retrospective study to assess 5-year outcomes among a large cohort of Medicare benificiaries undergoing sleeve gastrectomy and gastric bypass.
They found that “sleeve gastrectomy was associated with a lower risk of mortality, complications, reintervention, and other adverse events compared with gastric bypass up to 5 years after surgery. Despite these benefits, the rate of surgical revision at 5 years was higher for patients who underwent sleeve gastrectomy, and total health care spending was equivalent between groups…Overall, these results suggest that previously reported trends in early outcomes were sustained up to 5 years after surgery.”
In an editorial accompanying the study, Anita P. Courcoulas, MD, MPH, and Bestoun Ahmed, MD, both of the University of Pittsburgh Medical Center, concluded that Howard and colleagues “have succeeded in providing important incremental findings about the long-term comparative safety outcomes between bariatric procedures that will be helpful in clinical practice.” And that success, they explained, largely hinges on the study’s methodology.
Courcoulas and Ahmed explained that, without large-scale randomized trials, it is extremely difficult to “account for inherent bias in both patient and surgeon choice of procedure, when we know, for example, that in clinical practice, patients with diabetes and gastroesophageal reflux are directed more towards gastric bypass.”
To address this issue, Howard and colleagues used a method involving instrumental variables—using a variable that is correlated with the exposure (bariatric surgical procedure) but not associated with the outcome (safety)—in an attempt to mimic the random assignment of individuals to different procedures.
For their instrumental variable, the study authors used “the state-level rate of sleeve gastrectomy utilization among Medicare beneficiaries in the prior year (relative to gastric bypass).”
“In June 2012, the Centers for Medicare and Medicaid Services issued a National Coverage Determination (NCD) stating that ’effective for services performed on and after June 27, 2012, Medicare Administrative Contractors (MAC) acting within their respective jurisdictions may determine coverage of stand-alone laparoscopic sleeve gastrectomy (LSG) for the treatment of comorbid conditions related to obesity in Medicare beneficiaries,’” they explained. “We hypothesized that the decision to allow each MAC to make a Local Coverage Determination for its own respective jurisdiction would result in both geographic and temporal variation in the utilization of sleeve gastrectomy. This variation would then create the opportunity for a natural experiment in which treatment choice (sleeve gastrectomy vs gastric bypass) would be predicted to a large extent by whether a patient lived in a region with high or low sleeve gastrectomy utilization and would therefore be pseudorandom. This is similar to other studies that have successfully used variation in geographic factors as an instrumental variable.”
Courcoulas and Ahmed applauded this decision, noting that the “novel methods” used by the study authors allowed them to “creatively balance unmeasured factors…”
Howard and colleagues used their instrumental variable to estimate cumulative incidence of mortality, complications, and reinterventions up to 5-years after surgery among adult Medicare patients who underwent sleeve gastrectomy or gastric bypass from Jan. 1, 2012, through Dec. 31, 2018. Secondary outcomes included health care use after surgery, including hospitalization, emergency department use, and total spending.
The final study cohort consisted of 95,405 patients who underwent bariatric surgery—of these, 57,003 (60%) underwent sleeve gastrectomy (mean age, 57.1 years; 42,299 [74.2%] women; 124 [0.2%] Asian, 10,101 [17.7%] Black, 1,951 [3.4%] Hispanic, 314 [0.6%] North American Native; 43,194 [75.8%] White, 534 [0.9%] other, and 785 [1.4%] unknown) and 38,402 (40%) underwent gastric bypass (mean age, 55.9 years; 29,050 [75.7%] women; 109 [0.3%] Asian, 6,038 [15.7%] Black, 1,215 [3.2%] Hispanic, 278 [0.7%] North American Native, 29,986 [78.1%] White, 373 [1.0%] other, and 404 [1.1%] unknown).
“Compared with patients undergoing gastric bypass, at 5 years after surgery, patients undergoing sleeve gastrectomy had a lower cumulative incidence of mortality (4.27%; 95% CI, 4.25%-4.30% vs 5.67%; 95% CI, 5.63%-5.69%), complications (22.10%; 95% CI, 22.06%-22.13% vs 29.03%; 95% CI, 28.99%-29.08%), and reintervention (25.23%; 95% CI, 25.19%-25.27% vs 33.57%; 95% CI, 33.52%-33.63%),” Howard and colleagues wrote. “Conversely, patients undergoing sleeve gastrectomy had a higher cumulative incidence of surgical revision at 5 years (2.91%; 95% CI, 2.90%-2.93% vs 1.46%; 95% CI, 1.45%-1.47%).”
As for the secondary outcomes:
- The adjusted hazard ratio (aHR) for all-cause hospitalization and emergency department use was lower for patients who received sleeve gastrectomy at one year and three years, but not at five years:
- 1 year: Hospitalization, aHR 0.83 (95% CI, 0.80-0.86); ED use, aHR 0.87 (95% CI, 0.84-0.90).
- 3 years: Hospitalization, aHR 0.94 (95% CI, 0.90-0.98); ED use, aHR 0.93 (95% CI, 0.90-0.97).
- 5 years: Hospitalization, aHR 0.99 (5% CI, 0.94-1.04); ED use, aHR 0.97 (95% CI, 0.92-1.01).
- Total health care spending was lower among patients who received sleeve gastrectomy at 1 year post-surgery ($28,706 versus $30,663) but similar between groups at 3 years ($57,411 versus $58,581) and 5 years ($86,584 versus $85,762).
Despite the improved safety outcomes for sleeve gastrectomy, Howard and colleagues pointed out that total health care spending was only lower for the procedure in the first postoperative year, a cost equivalency that was corroborated in previous studies.
“Insofar as adverse events drive health care spending, one might expect the lower cost of sleeve gastrectomy to be sustained for all 5 years,” they wrote. “Therefore, there may be other drivers of health care spending not under examination in the current study that account for this lack of a difference.”
Howard and colleagues concluded that longer-term randomized clinical trials and observational studies “are warranted to confirm these findings. Understanding the risk profile of various bariatric operations may further help patients and surgeons make the most appropriate decisions regarding plans of care.”
Study limitations include using Medicare claims to create the study cohort, which may limit generalizability; a lack of clinical granularity in claims data; and the study’s observational, non-randomized design.
-
Patients who underwent sleeve gastrectomy had better 5-year outcomes for long-term mortality, complications, and reinterventions compared with gastric bypass, but they were also more likely to need surgical revision.
-
Patients receiving sleeve gastrectomy had lower total health care spending in the first postoperative year compared to gastric bypass, but not at 3 or 5 years post-surgery.
John McKenna, Associate Editor, BreakingMED™
Howard reported funding from the Blue Cross Blue Shield of Michigan Foundation and the National Institute of Diabetes and Digestive and Kidney Diseases.
Courcoulas reported grants from the National Institutes of Health, the National Institute of Diabetes and Digestive and Kidney Diseases, Patient-Centered Outcomes Research Institute, and Allurion Inc. outside the submitted work.
Cat ID: 518
Topic ID: 86,518,282,494,730,795,518,917,925