Isolated small fiber neuropathy (SFN) is uncommon, but its incidence may be growing, a retrospective study suggested.
“Most patients do not develop major neurological impairments and disability but have multiple comorbidities, including cardiovascular ischemic events, and increased mortality from SFN onsets,” wrote Christopher Klein, MD, of Mayo Clinic in Rochester, Minnesota, and co-authors in Neurology.
“Development of large fiber involvements and diabetes are common over time,” they continued. “Targeted testing facilitates interventional therapies for diabetes but also rheumatologic and rare genetic forms.”
Between January 1998 and December 2017, the researchers identified 94 patients with SFN in Olmsted, Minnesota, or nearby counties, based on symptoms (pain, burning, sensory loss, and autonomic changes) and testing that included thermoregulatory sweat, quantitative sudomotor axon reflex, and quantitative sensory tests.
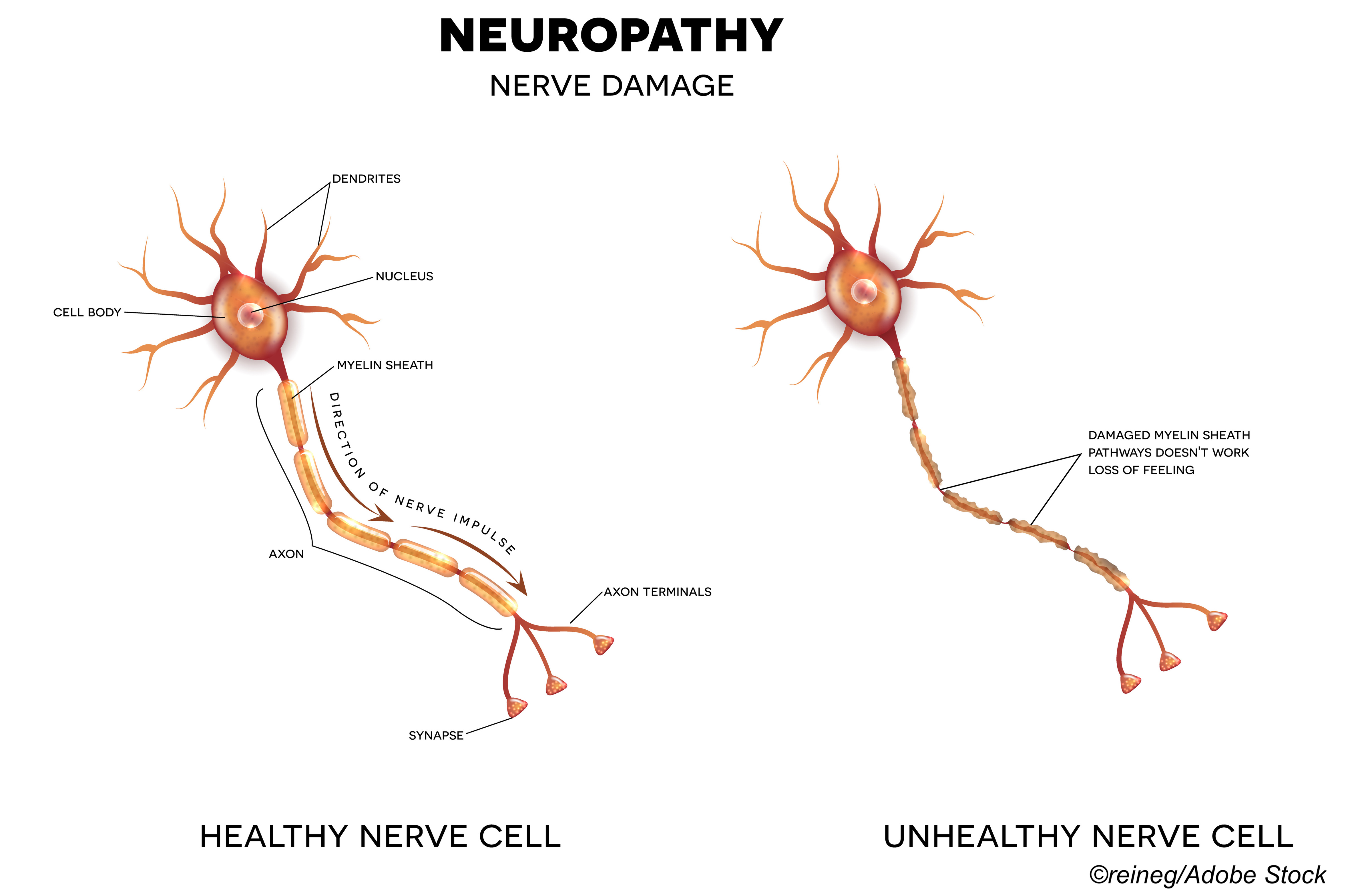
Because electrodiagnostic tests—electromyography and nerve conduction—assess mainly large fibers, patients with significant findings on these tests were excluded. SFN patients were compared with 282 sex- and age-matched controls with no diagnosis of SFN or any other neuropathy. Average follow-up was 6.1 years.
Incident SFN was 1.3/100,000/year and increased over the study, with prevalence 13.3/100,000, Klein and colleagues reported.
“Incidence of SFN was much lower compared to the earlier report from the Netherlands, but different methodologies were utilized,” they said. “In contrast we did not exclude individuals <20 years of age, examined a 20-year period (SFN quantitative testing readily available at our institution throughout this time), and excluded patients with SFN who died in our prevalence calculations.”
People with SFN had a mean onset age of 54 and 67% were female. Idiopathic SFN was the most common diagnosis (70%), followed by SFN related to diabetes (15%), Sjögrens (2%), AL-amyloid (1%), transthyretin-amyloid (1%), Fabry (1%), lupus (1%), post viral (1%), Lewy body (1%), and multifactorial reasons (5%).
For SFN patients versus controls, respectively, there were higher rates of:
- Obesity (BMI mean 30.4 versus 28.5).
- Insomnia (86% versus 54%).
- Opioid prescriptions (72% versus 46%).
- Non-opioid pain prescriptions (67% versus 18%).
- Hypertriglyceridemia (180 mg/dl mean versus 147 mg/dl).
- Diabetes mellitus (diabetes; 51% versus 22%).
There was no difference in history of substance abuse or psychiatric illness between the groups.
Patients with SFN did not self-identify as disabled and had a median modified Rankin Scale score of 1.0 (range 0-6; higher implies more disability; 1 implies symptoms that do not interfere with daily activities). For controls, the median score was 0 (no symptoms, P difference=0.04)
Measures of autonomic function and disability progression showed modest change for most etiologies. For onset Composite Autonomic Severity Score (CASS; scores of >7 indicate autonomic impairment) the median score was 3, and change/year was 0.08 (range 0-2.0). The median Neuropathy Impairment Score (NIS) was 2 at onset (range 0 to 8) with change/year of 1.0 (range −7.9 to +23.3). Faster progression, with NIS and CASS change >+1 point/year occurred only in AL-amyloid, hereditary transthyretin-amyloid, Fabry, uncontrolled diabetes, and Lewy body etiologies.
Myocardial infarctions were more common in those with SFN (46%) versus controls (27%, P<0.0001). Mean age at death was not significantly different (70 versus 73, P=0.55), but death from symptom onset was higher in patients with SFN (19%) versus controls (12%, P<0.001).
“Not only were pure SFN patients more likely to take opioids and have issues with sleep, but they were also more likely to have heart attacks and to die,” observed Brian Callaghan, MD, MS, of University of Michigan, Ann Arbor, and J. Robinson Singleton, MD, of University of Utah, Salt Lake City, in an accompanying editorial.
“Disease modifying therapies are needed to prevent heart attacks and death as well as the pain that likely leads to opioid use and poor sleep in this population,” Callaghan and Singleton added. “Treatment of metabolic risk factors is one potential intervention.”
“Fast progression was only seen in patients with amyloidosis, uncontrolled diabetes, or Lewy body dementia,” they noted. “Therefore, patients with SFN can be counseled that progression and disability are likely to be modest in most cases. However, when patients do progress quickly, uncommon etiologies should be sought.”
Consensus diagnostic criteria for idiopathic neuropathies including distal sensory polyneuropathy, mixed fiber sensory neuropathy, small fiber sensory neuropathy, and large fiber sensory neuropathy were published in 2020. Criteria for idiopathic small fiber sensory neuropathy required one or more small fiber symptom, one or more small fiber sign, and abnormal distal intraepidermal nerve fiber density biopsy findings, with normal sensory nerve conduction studies and no large fiber symptoms or signs.
“Limitations of electrodiagnostic testing and limited examination findings may be the reason that neurologists have focused primarily on neuropathies with mixed or large fiber involvement,” the editorialists noted. “A more recent diagnostic procedure, 3 mm punch skin biopsies analyzed for nerve fiber density in the epidermis, quantitates distal small fiber nerve injury, and has led to a new focus on isolated SFN.”
Limitations of the present study include its population drawn from Olmsted, Minnesota, and nearby areas, which may limit its generalizability.
“The primary limitation of this study is its retrospective nature,” Klein and co-authors acknowledged. “Prospective studies examining all patients presenting with symptoms of small fiber neuropathy, utilizing detailed histories, exams, and a battery of quantitative measures of small fiber dysfunction are needed to confirm our findings.”
-
A retrospective study by Mayo Clinic researchers suggested incidence of isolated small fiber neuropathy (SFN) may be growing.
-
Be aware that rapid progression of SFN was only observed in patients with amyloidosis, uncontrolled diabetes, or Lewy body dementia.
Paul Smyth, MD, Contributing Writer, BreakingMED™
This study was funded by the Mayo Clinic Foundation, Mayo Clinic Center of Individualized Medicine, Mayo Clinic Center of MS, and Autoimmune Neurology.
Klein has received teaching honorarium from Ackea pharmaceuticals for lectures on hereditary transthyretin amyloidosis and Fabry disease. He has consulted for Pfizer regarding tafamidis (all compensation for consulting activities is paid directly to Mayo Clinic) and participated in the clinical trials for inotersen and patisiran but received no personal compensation for his participation.
Callaghan consults for DynaMed, performs medical legal consultations including consultations for the Vaccine Injury Compensation Program, and receives research support from the American Academy of Neurology. Singleton has consulted for Regenacy.
Cat ID: 130
Topic ID: 82,130,730,358,914,130,192,925