Recurrent strokes significantly increased the relative risk for dementia, according to findings from an observational study, which also linked increased risk for dementia with stroke severity.
Compared with participants who never had a stroke, risk of dementia was HR 1.73 (95% CI 1.49-2.00) for people with one minor to mild stroke, 3.47 (95% CI 2.23-5.40) for one moderate to severe stroke, 3.48 (95% CI 2.54-4.76) for two or more minor to mild strokes, and 6.68 (95% CI 3.77-11.83) for two or more moderate to severe strokes, after adjusting for sociodemographic characteristics, apolipoprotein E status, and vascular risk factors, reported Silvia Koton, PhD, RN, of Tel Aviv University in Israel, and co-authors.
Adjusted incidence rates of dementia were 0.47 (95% CI 0.44-0.50) for people without stroke and 1.21 (95% CI 1.05-1.40) for people with stroke, the researchers wrote in JAMA Neurology.
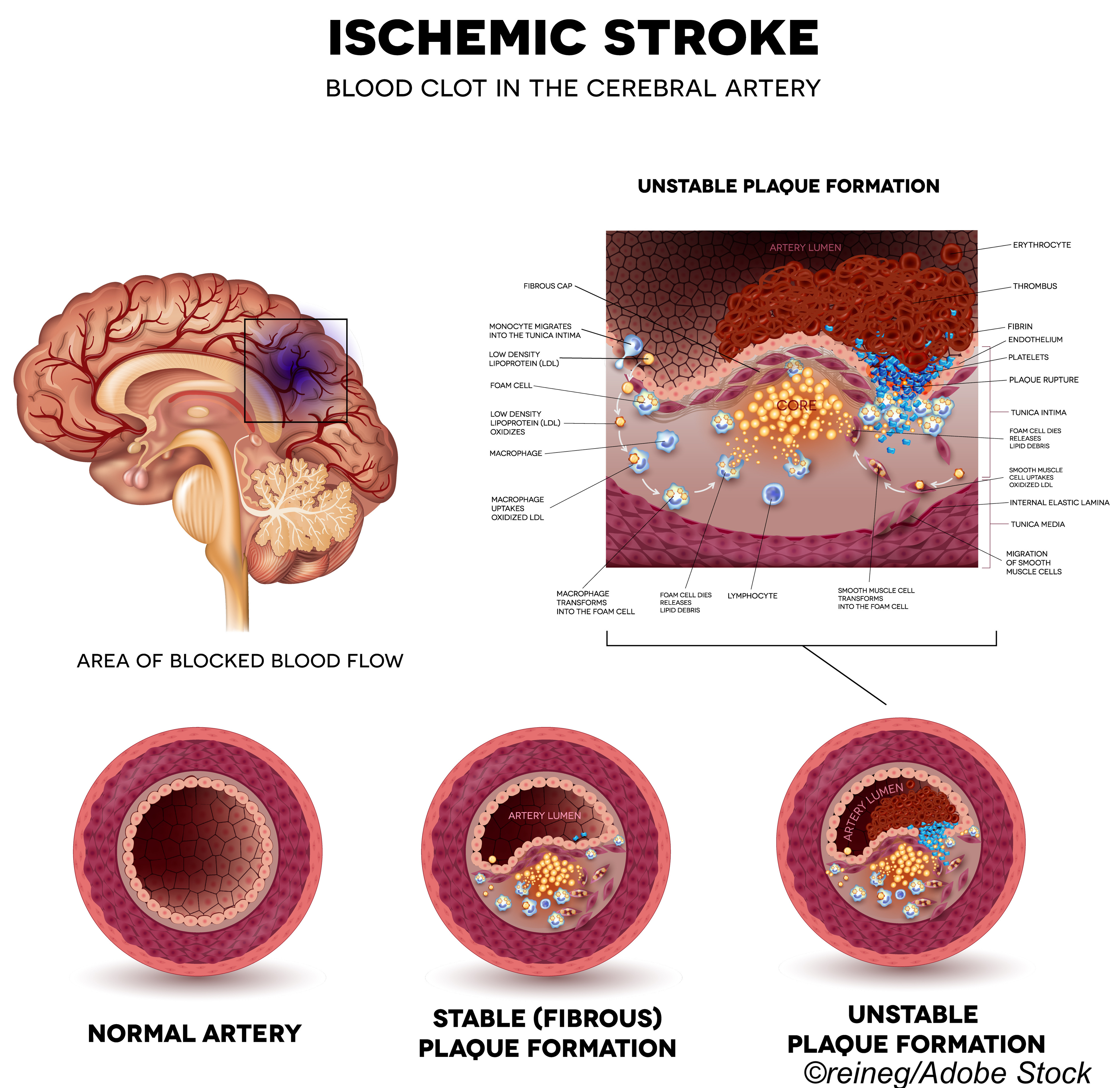
“In this study, risk of dementia significantly increased after ischemic stroke, independent of vascular risk factors,” Koton and co-authors wrote. “Results suggest a dose-response association of stroke severity and recurrence with risk of dementia.”
“Risk of stroke, and thus recurrent stroke and dementia, is increased in individuals with more vascular risk factors,” the researchers noted. “An estimated 39% of recurrent strokes and 10% of post-stroke dementia cases are attributable to vascular risk factors present before the stroke. By evaluating these risk factors and their changes and treatment over time, we demonstrated that the risk of dementia was elevated independent of these risk factors for both first and recurrent strokes.”
“These data emphasize the value of both primary and secondary stroke prevention for reducing dementia risk,” they added
The findings are both expected and surprising, noted Deborah Levine, MD, MPH, of the University of Michigan in Ann Arbor, who was not involved with the study. “In a racially diverse sample, this rigorous study confirms that stroke roughly doubles dementia risk, and dementia risk is higher in adults who suffer more severe strokes and recurrent strokes,” she wrote in an email to BreakingMED.
“Surprisingly, vascular risk factors before and after stroke did not explain the risk of post-stroke dementia. It is also surprising that Black adults had a higher risk of dementia after moderate to severe stroke than White adults,” Levine observed.
While previous studies of post-stroke dementia risk had mostly White populations and could not control for pre-stroke cognition, this study “included Black and White adults and controlled for pre-stroke cognition. So, the findings are robust and generalizable,” she continued.
Clinicians need to monitor stroke survivors closely for cognitive decline after stroke, Levine noted: “Preventing stroke is a potential strategy for reducing dementia risk,” she wrote.
Researchers studied 15,379 patients in the ongoing Atherosclerosis Risk in Communities (ARIC) study who were free of stroke and dementia at baseline (1987 to 1989) with follow-up through December 2019. Mean baseline age was 54.1 and 55.2% were women. Overall, 73.3% of participants were White and 26.7% were Black.
The relationship between dementia and ischemic stroke incidence, frequency, and severity was determined over median follow-up of 25.5 years and a mean of 4.4 visits for evaluation. Data about atrial fibrillation, diabetes, use of anti-hypertensives or statins, and smoking status were updated during follow-up. For participants with stroke, dementia incidence in the first year after stroke was not counted to eliminate transient cognitive changes.
Among 1,155 incident strokes identified in follow-up, severity was classified by the National Institutes of Health Stroke Scale (NIHSS) as minor (NIHSS 5 or less, 62.8%); mild (NIHSS 6-10, 22.1%); moderate (NIHSS 11-15, 7.9%); or severe (NIHSS 16 or more, 7.1%).
Dementia was diagnosed in 2,860 cases, which included those with incident stroke diagnosed 1 year or more after the stroke, as well as dementia diagnosed any time after baseline in those without stroke. Of the total, 24.1% were diagnosed through in-person evaluation, 30.5% via telephone assessment, 36.5% through hospital records, and 9% through death records.
There were 269 preceding ischemic strokes among the 2,860 participants with dementia, and median time from ischemic stroke to incident dementia was 7.2 years. For participants with stroke, the proportion of dementia risk attributable to stroke was 17.4% (95% CI 4.8 to 28.6), which increased with frequency (9.1% for one stroke vs 53.0% for two or more strokes) and severity (7% for NIHSS ≤5 vs 50% for NIHSS ≥16).
After adjusting for risk factors, increased hazard rates of dementia were associated with stroke frequency (increasing from 1.81 for one event to 3.91 for two or more events) and severity (1.79 for NIHSS ≤5 to 4.70 for NIHSS ≥16). Age without dementia at median survival significantly decreased from 90 years in participants without stroke to 81.3 in those with minor to mild stroke and to 73.8 in those with moderate to severe stroke.
“There was a statistically significant interaction between race and moderate to severe stroke with a stronger adjusted relative hazard of dementia among Black participants with a moderate to severe stroke,” the authors noted.
Limitations of the study include the possibility of bias due to attrition and survivorship. The researchers also acknowledged that measures of comorbidity and medication use are not comprehensive markers of risk-factor control, and the possibility of residual confounding exists in the analysis. In addition, data on stroke severity were not prospectively assessed in ARIC and severity information was based on hospitalization records; exact time of evaluation after stroke onset was not available.
Disclosure:
The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts.
Koton reported no disclosures.
Levine reported no disclosures.
by
Paul Smyth, MD, Contributing Writer, BreakingMED™
Kaiser Health News
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation, which is not affiliated with Kaiser Permanente.