Cyst-size by itself was not reliable for estimating the progression risk for pancreatic pre-neoplastic lesions, but other factors, such as patient BMI, can be more useful, researchers reported.
In over 500 patients with branch-duct intraductal papillary mucinous neoplasms (BD-IPMNs) who were under surveillance for about 4 years, initial cyst size >15 mm, body BMI >26.4 kg/m2, and heavy smoking were linked with progression risk of BD-IPMNs, as was the AA blood genotype, according to Paolo Giorgio Arcidiacono, MD, of the San Raffaele Scientific Institute IRCCS in Milan, and co-authors.
However, cyst size, along with the others factors, “is helpful for planning personalized surveillance of BD-IPMNs,” they wrote in JAMA Network Open.
The authors explained that “When IPMNs harbor morphologic features associated with cancer risk, surgery is indicated, and surveillance is advised for most patients with good life expectancy.”
Guidelines for IPMN management, such as those from the International Association of Pancreatology and the American Gastroenterology Association (AGA), emphasize the importance of specific morphologic features tied to a higher cancer risk, and those include size of the BD cyst, presence of solid nodules, and main pancreatic duct dilation.
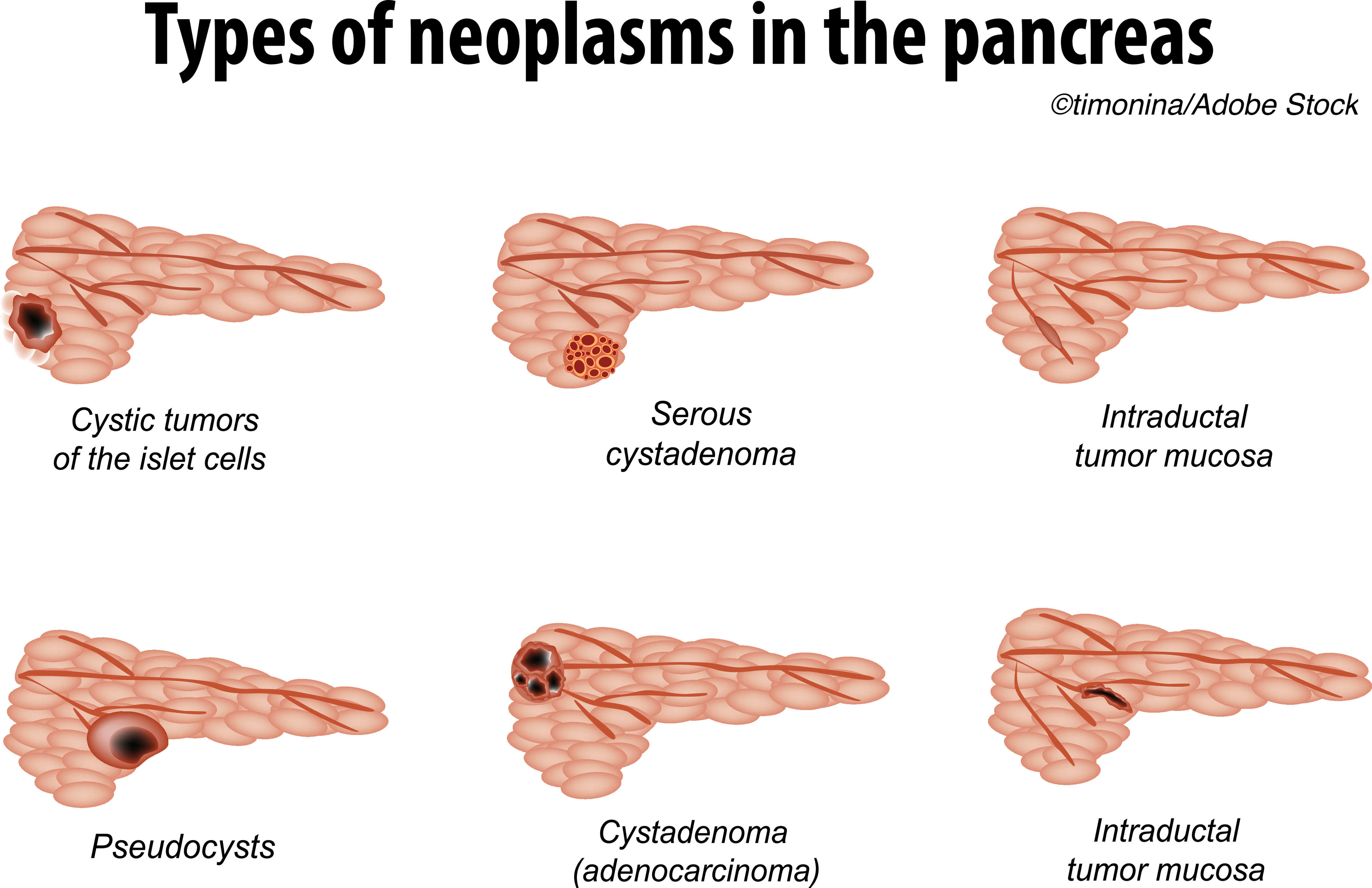
“Most IPMNs, however, are small BD lesions without such features and carry a low risk of cancer,” Arcidiacono’s group wrote; so, they sought to “investigate comprehensively cyst-related and patient-related factors associated with worrisome features (WFs) or high-risk stigmata (HRS) development in a cohort of BD-IPMNs under surveillance.”
They evaluated cyst-related and patient-related factors of consecutive BD-IPMNs, without WFs or HRS, in patients in Italy diagnosed from 2009 to 2018 with at least 12 months’ surveillance until Feb 2020. Patients (median age 66; 62.4% women) were registered in a two-center ambispective (prospective and retrospective components) cohort study. The study endpoint was the progression to WFs or HRS, whichever occurred first. The authors also looked at the ABO blood group in a substudy.
In terms of the exclusion criteria, Arcidiacono’s group noted that WFs were defined by several elements including a ≥3 cm cyst size, enhancing mural nodule <5 mm, main pancreatic duct size between 5 and 10 mm, lymphadenopathy, increased serum cancer antigen 19-9 (CA-19-9) level, and acute pancreatitis. Also, the defining factors for HRI were IPMNs causing obstructive jaundice, enhancing mural nodules ≥5 mm, and main pancreatic duct ≥10 mm.
Among 540 patients with BD-IPMNs who were observed for a median of 51.5 months for 2,758 person-years, 24.1% experienced progression. The probability of progression was 3.7% at 1 year, 23.4% at 5 years, and 43.3% at 10 years, according to the authors. Additionally, 2.8% of the patients underwent surgery, 1.3% had malignant histologic findings, and 0.56% died of pancreatic-associated disease.
Arcidiacono and co-authors reported the following hazard ratios for the “significant independent factors associated with progression risk:”
- Initial cyst size >15 mm: HR 2.05 (95% CI 1.44 to 2.91).
- BMI >26.4 kg/m2: HR 1.72 (95% CI 1.19 to 2.50).
- Heavy smoking: HR 1.81 (95% CI 1.14 to 2.86).
- AA blood genotype vs OO genotype: HR 3.49 (95% CI 1.04 to 11.71).
The last finding “strengthens the hypothesis of the O allele to be protective against PDAC [pancreatic ductal adenocarcinoma] development and confirms a more relevant role of the A group,” the authors wrote.
They found also that the median time to development of either WFs or HRS was 45 months, and that the rate of progression to either a WF or an HRS during surveillance was 47.1/1,000 person-years or 4.7% per year, with 30.7% occurring after 5 years of stable findings.
While the study had limitations — no “hard outcomes” such as “death or disease that may cause death;” lack of prospective measure of CA-19-levels; and the exploratory nature of the blood-groups study – Arcidiacono’s group emphasized that, given their results, clinicians “need to consider with caution the [AGA] 2015 guideline recommendations to discontinue surveillance of BD-IPMNs after 5 years of no significant changes.”
In an invited commentary accompanying the study, J.-Matthias Löhr, MD, PhD, of the Karolinska Institutet in Stockholm, and Marco Del Chiaro, MD, PhD, of the University of Colorado-Anschutz Medical Campus in Denver, stressed the benefit of the finding beyond dollars and cents: “The potential impact of this finding can be relevant: to have a simple way to distinguish those in need of surveillance from those who have less risk to progress may have consequences… will also relieve many of these patients with incidental findings from the burden of a potentially life-threatening disease – or major pancreatic surgery carrying its own rate of morbidity and mortality and impact on quality of life.”
However, Löhr and Del Chiaro pointed out that the study was saddled with “2 unavoidable biases that occur in every study involving a population of patients with IPMN under surveillance,” namely that “the accuracy in diagnosis of cystic lesions is not very high,” and “the actual goal of IPMN treatment is to catch high-grade dysplasia.”
“Theoretically, we should be able to investigate predictor factors of high-grade dysplasia, but unfortunately, we do not yet have any clinical or diagnostic tools able to achieve this goal,” they wrote.
Two studies that are currently recruiting, one on radiogenomics to predict the malignancy potential of IPMN of the pancreas and the other on the molecular detection of advanced neoplasia in pancreatic cysts, may offer some more answers.
-
Cyst size alone was not a reliable factor to estimate progression risk in branch-duct intraductal papillary mucinous neoplasms (BD-IPMNs), but along with other readily available data, size may prove helpful for planning personalized surveillance of BD-IPMNs.
-
Initial cyst size >15 mm, body BMI, heavy smoking, and AA blood genotype were tied to progression risk of BD-IPMNs.
Shalmali Pal, Contributing Writer, BreakingMED™
Arcidiacono reported no relationships relevant to the contents of this paper to disclose. Co-authors reported suppport from the American International Recruitment Council and a Gioja Bianca Costanza Legacy donation.
Löhr reported no relationships relevant to the contents of this paper to disclose. Del Chiaro reported support from Boston Scientific and Haemonetics.
Cat ID: 112
Topic ID: 77,112,187,112,188,120,935,192,925