More than 80% of patients with chronic kidney disease (CKD) who underwent aortic valve replacement showed stable or improved kidney function a month later, according to a single-center study from Israel.
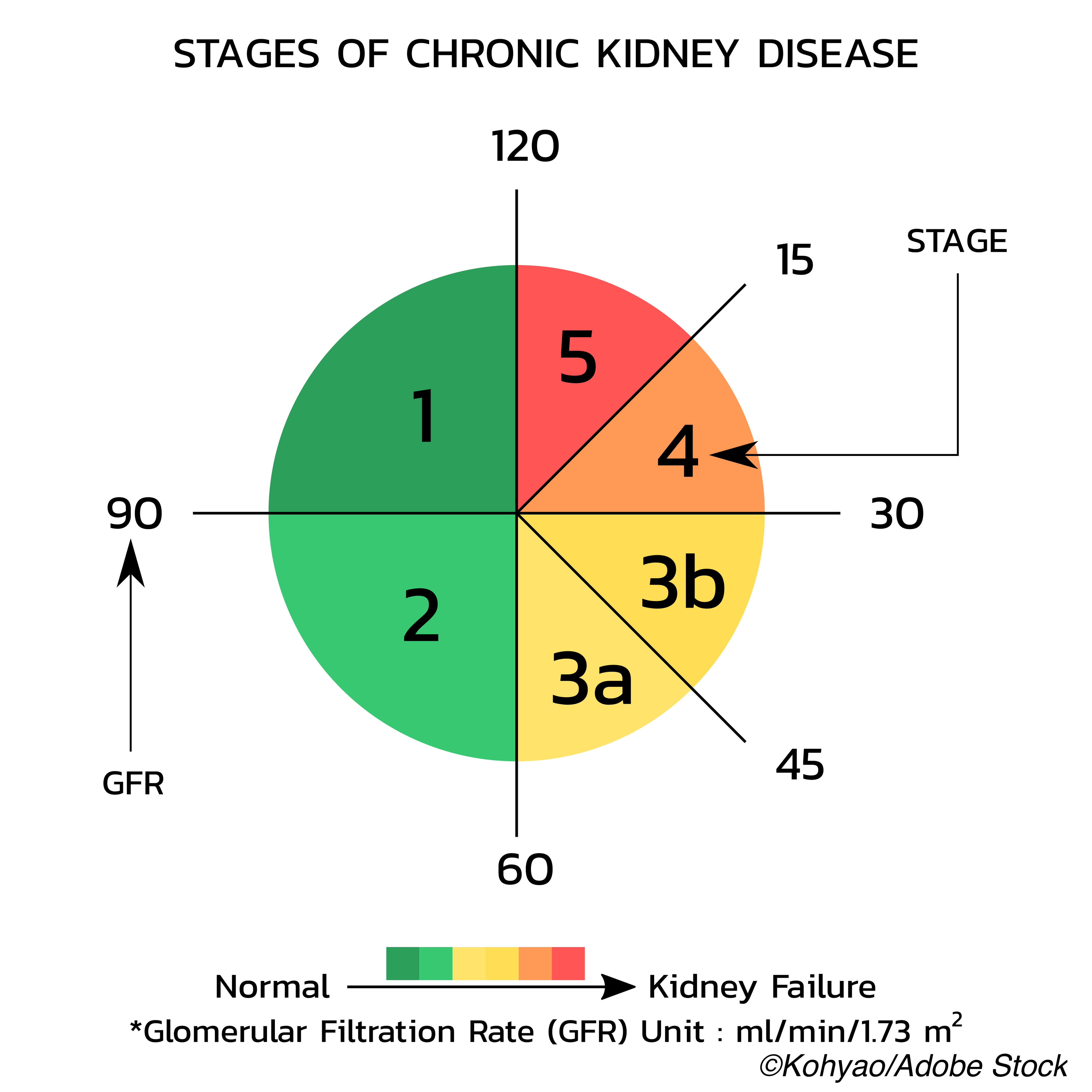
In a retrospective, cohort study performed from 2008 to 2019, CKD stage remained stable or improved in 80.6% of the 894 patients enrolled, with only 0.97% progressing to stage 5 CKD one month after transcatheter aortic valve replacement (TAVR), reported Guy Witberg, MD, of Rabin Medical Center-Beilinson Hospital in Petach Tikva, Israel, and co-authors.
In addition, acute kidney injury (AKI) occurred in 11.1% of patients in stage 1 and in 48.7% of those in stage 2 by 48 hours, and 63.5% of those cases had resolved by discharge. Further, one month after TAVR, estimated glomerular filtration rate (eGFR) improved by at least 10% in 36.8% and deteriorated by at least 10% in 26.1%, they reported in JAMA Network Open.
Finally, Witberg and colleagues found that kidney function improvement was favorably associated with two-year mortality, but they warned of one unfavorable finding: “deterioration in kidney function was associated with increased mortality regardless of baseline CKD status.”
They cited two main take-home clinical messages from the study: Reassurance on the safety of TAVR for kidney outcomes in the general population and in those with aortic stenosis (AS) and CKD, and the “importance of deterioration in kidney function after TAVR, either periprocedural or at steady state,” as well as the need to “prevent kidney injury in patients undergoing TAVR regardless of baseline renal function.”
The results by Witberg’s group on the “progressive intertwined death spiral of both the heart and the kidney,” is in line with previous research, such as a 2011 retrospective review of >2,000 aortic valve replacement patients with cardiorenal dysfunction and a 2017 substudy of the PARTNER 1 Trial and Registry, pointed out Benjamin Z. Galper, MD, MPH, of Mid-Atlantic Permanente Medical Group in McLean, Virginia, in an invited commentary accompanying the study.
But Witberg et al also offer novel data on the “complex interplay between TAVR and CKD,” Galper added. For instance, patients who normalized their eGFR to >60 mL/min/1.73 m2 had the same death rate as patients undergoing TAVR without CKD. “If this finding is replicated in larger, multicenter trials, it would demonstrate that TAVR could cure cardiorenal syndrome,” he noted.
Galper re-emphasized the cautionary note from Witberg and co-authors that “worsening kidney function in patients undergoing TAVR could lead to increased mortality and that steps should be taken to prevent AKI and worsening CKD after TAVR.”
The study was done at a public, tertiary academic medical center that is a regional referral center for valvular heart interventions, the authors explained. Consecutive cases of patients undergoing TAVR were included in the study, with available baseline and post-TAVR data on kidney function. Patients were excluded if they had hemodialysis, no serum creatinine data at discharge or at one month, or died in-hospital or within one month of discharge. Mean patient age was 82.2 years, and 51.2% were women.
Of those patients, 40.5% were treated from 2017 to 2019, 38.9% from 2013 to 2016, and 20.5% from 2008 and 2012. Patients had a mean Society of Thoracic Surgeons (STS) score of 5.2% and a mean eGFR of 65.1 mL/min/1.73 m2. The study’s main outcome was overall mortality at 2-year follow-up.
Witberg’s group explained that “we do not perform percutaneous coronary interventions (PCI) concomitantly with TAVR in order to minimize contrast exposure. When significant coronary disease with a clear indication for revascularization is discovered during the workup for TAVR, patients are scheduled for elective PCI, usually at least 2 weeks before the scheduled TAVR. [TAVR] is performed only after reassessment of kidney function to determine that it has not deteriorated after PCI.”
They reported that a deterioration of ≥10% in eGFR one month after TAVR was tied to a hazard ratio of 2.16 (95% CI 1.24 to 5.24, P=0.04) at two-year mortality. As Galper pointed out, “[p]atients who showed CKD status resolution (eGFR improvement to >60 mL/min/1.73 m2 after TAVR) had a similar 2-year mortality to those with baseline eGFR greater than 60 mL/min/1.73 m2 and vice versa,” they wrote.
Factors associated with steady state kidney function deterioration were:
- STS >6%: odds ratio (OR): 1.43 (95% CI 1.03-1.98, P=0.03).
- baseline eGFR >75 mL/min/1.73 m2: OR: 1.92 (95% CI 1.40-2.62, P=0.0013).
- Higher AKI during 48 hours after TAVR: OR: 2.82 (95% CI 1.70-4.70, P<0.001); OR: 7.32 if not resolved by discharged (95% CI 4.53-11.42, P<0.001).
Factors linked with steady state kidney function improvement after TAVR were:
- Female sex: OR: 1.27 (95% CI 1.03-1.61, P=0.04).
- eGFR <60 mL/min/1.73 m2: OR: 2.28 (95% CI 1.73-3.01, P=0.004).
- Higher baseline left ventricular ejection fraction: 56.1% for stable eGFR, 56.6% for eGFR improvement, 55.7% for eGFR deterioration (P=0.47).
- Lower contrast-eGFR ratio: mean: 2.5, mean: 3.1, mean: 3.3, respectively (P=0.01)
In terms of the results seen in female patients, Gasper noted that “female sex is more likely to be associated with cardiorenal syndrome, [but] we must invest in efforts to better determine risk factors and diagnostic criteria…to be able to detect cardiorenal syndrome at earlier stages in patients with AS,” while the authors stated that “because women undergoing TAVR tend to have a lesser comorbidity burden compared with men, it is reasonable to assume that [cardiorenal syndrome] was more prevalent as a cause for kidney dysfunction in women as compared with men, which would explain their higher likelihood for improvement in kidney function after TAVR.”
The authors also found that rates of periprocedural vascular and bleeding complications were higher in patients who developed AKI, while the need for pacemaker implantation was similar between patients with or without AKI, and “there was no difference in vascular complications, bleeding complications, or the need for pacemaker implantation between patients with steady state stable, improved, or deteriorated kidney function.”
Study limitations included its single-center, observational and retrospective design; the inability to assess the association of concomitant PCI during TAVR with either kidney function or survival after TAVR; the evaluation of steady state renal function only at 1 month after TAVR; and the study period of 11 years, “during which many changes and advances in the practice of TAVR occurred in terms of the procedure itself as well as patient selection and postprocedural care; therefore, not all patients included in the study could be considered to represent current clinical practice.”
Nonetheless, Witberg and co-authors emphasized that “When examining the factors found to be associated with deterioration in kidney function or change in CKD status after TAVR, our results highlight the importance of minimizing contrast exposure and prevention of AKI… Although other factors associated with new CKD status or deterioration in kidney function after TAVR cannot be modified… minimizing contrast exposure can be promoted by… lower rates of injections, using ultrasound guidance to avoid the need for angiography to guide the femoral puncture, fusion imaging to replace aortograms for placement of the device, and echocardiographic assessment of perivalvular leaks instead of using postimplantation aortogram.”
-
Transcatheter aortic valve replacement (TAVR) proved safe in terms of kidney outcomes and has the potential to improve kidney function in patients with chronic kidney disease; however, kidney injury should be prevented in patients undergoing TAVR regardless of baseline renal function.
-
Kidney function improved or remained stable in the vast majority of study patients one month after TAVR, while steady state kidney function had a stronger association with mortality than did baseline kidney function.
Shalmali Pal, Contributing Writer, BreakingMED™
Witberg reported no relationships relevant to the contents of this paper to disclose. A co-author reported relationships with Fresenius Medical Care and AstraZeneca.
Galper reported no relationships relevant to the contents of this paper to disclose.
Cat ID: 308
Topic ID: 74,308,730,308,914,127,192,925,492


